Ayse S. Cakmak
Late fusion of machine learning models using passively captured interpersonal social interactions and motion from smartphones predicts decompensation in heart failure
Apr 04, 2021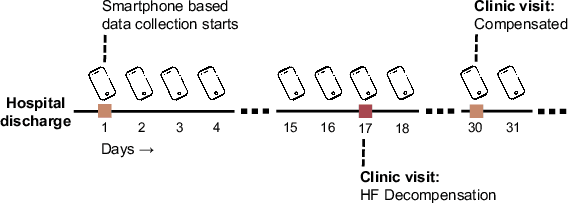
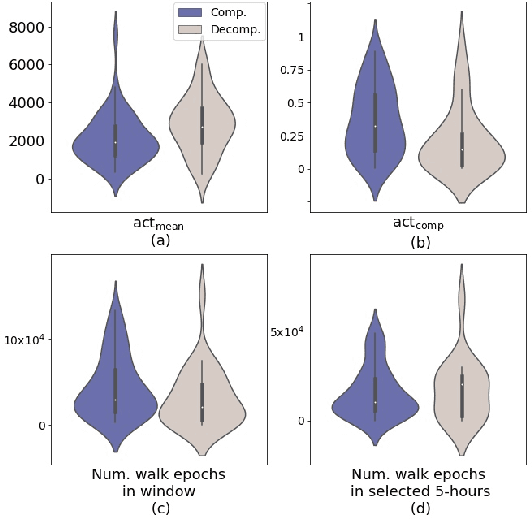
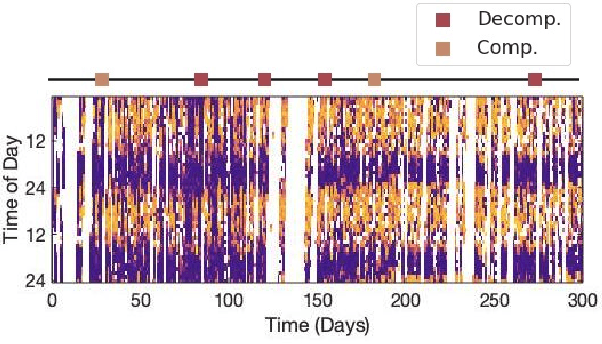
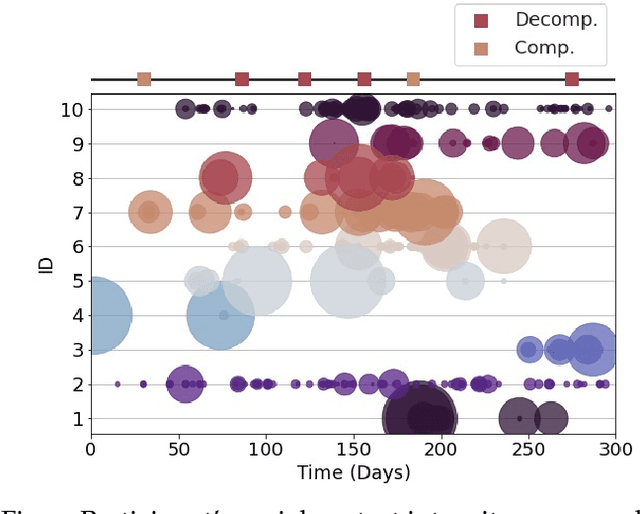
Abstract:Objective: Worldwide, heart failure (HF) is a major cause of morbidity and mortality and one of the leading causes of hospitalization. Early detection of HF symptoms and pro-active management may reduce adverse events. Approach: Twenty-eight participants were monitored using a smartphone app after discharge from hospitals, and each clinical event during the enrollment (N=110 clinical events) was recorded. Motion, social, location, and clinical survey data collected via the smartphone-based monitoring system were used to develop and validate an algorithm for predicting or classifying HF decompensation events (hospitalizations or clinic visit) versus clinic monitoring visits in which they were determined to be compensated or stable. Models based on single modality as well as early and late fusion approaches combining patient-reported outcomes and passive smartphone data were evaluated. Results: The highest AUCPr for classifying decompensation with a late fusion approach was 0.80 using leave one subject out cross-validation. Significance: Passively collected data from smartphones, especially when combined with weekly patient-reported outcomes, may reflect behavioral and physiological changes due to HF and thus could enable prediction of HF decompensation.
Using Convolutional Variational Autoencoders to Predict Post-Trauma Health Outcomes from Actigraphy Data
Nov 20, 2020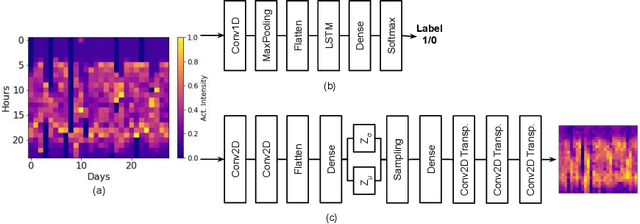
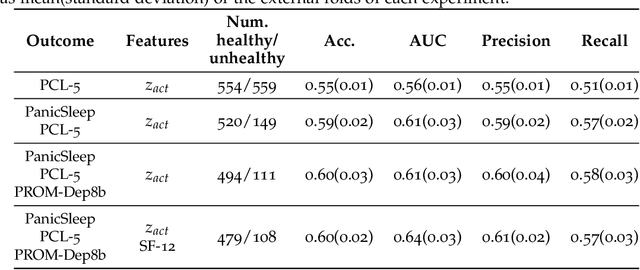
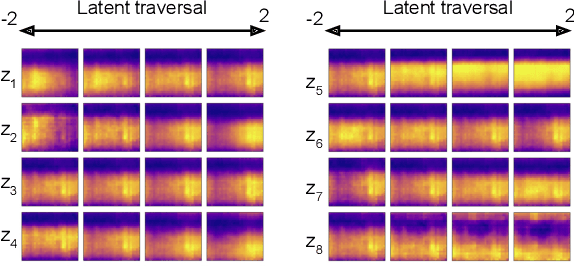
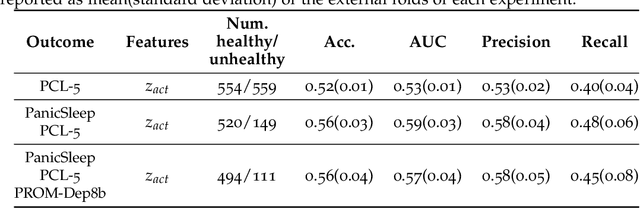
Abstract:Depression and post-traumatic stress disorder (PTSD) are psychiatric conditions commonly associated with experiencing a traumatic event. Estimating mental health status through non-invasive techniques such as activity-based algorithms can help to identify successful early interventions. In this work, we used locomotor activity captured from 1113 individuals who wore a research grade smartwatch post-trauma. A convolutional variational autoencoder (VAE) architecture was used for unsupervised feature extraction from four weeks of actigraphy data. By using VAE latent variables and the participant's pre-trauma physical health status as features, a logistic regression classifier achieved an area under the receiver operating characteristic curve (AUC) of 0.64 to estimate mental health outcomes. The results indicate that the VAE model is a promising approach for actigraphy data analysis for mental health outcomes in long-term studies.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge