Wenchao Guo
STARS: Shared-specific Translation and Alignment for missing-modality Remote Sensing Semantic Segmentation
Jan 24, 2026Abstract:Multimodal remote sensing technology significantly enhances the understanding of surface semantics by integrating heterogeneous data such as optical images, Synthetic Aperture Radar (SAR), and Digital Surface Models (DSM). However, in practical applications, the missing of modality data (e.g., optical or DSM) is a common and severe challenge, which leads to performance decline in traditional multimodal fusion models. Existing methods for addressing missing modalities still face limitations, including feature collapse and overly generalized recovered features. To address these issues, we propose \textbf{STARS} (\textbf{S}hared-specific \textbf{T}ranslation and \textbf{A}lignment for missing-modality \textbf{R}emote \textbf{S}ensing), a robust semantic segmentation framework for incomplete multimodal inputs. STARS is built on two key designs. First, we introduce an asymmetric alignment mechanism with bidirectional translation and stop-gradient, which effectively prevents feature collapse and reduces sensitivity to hyperparameters. Second, we propose a Pixel-level Semantic sampling Alignment (PSA) strategy that combines class-balanced pixel sampling with cross-modality semantic alignment loss, to mitigate alignment failures caused by severe class imbalance and improve minority-class recognition.
MSSDF: Modality-Shared Self-supervised Distillation for High-Resolution Multi-modal Remote Sensing Image Learning
Jun 11, 2025
Abstract:Remote sensing image interpretation plays a critical role in environmental monitoring, urban planning, and disaster assessment. However, acquiring high-quality labeled data is often costly and time-consuming. To address this challenge, we proposes a multi-modal self-supervised learning framework that leverages high-resolution RGB images, multi-spectral data, and digital surface models (DSM) for pre-training. By designing an information-aware adaptive masking strategy, cross-modal masking mechanism, and multi-task self-supervised objectives, the framework effectively captures both the correlations across different modalities and the unique feature structures within each modality. We evaluated the proposed method on multiple downstream tasks, covering typical remote sensing applications such as scene classification, semantic segmentation, change detection, object detection, and depth estimation. Experiments are conducted on 15 remote sensing datasets, encompassing 26 tasks. The results demonstrate that the proposed method outperforms existing pretraining approaches in most tasks. Specifically, on the Potsdam and Vaihingen semantic segmentation tasks, our method achieved mIoU scores of 78.30\% and 76.50\%, with only 50\% train-set. For the US3D depth estimation task, the RMSE error is reduced to 0.182, and for the binary change detection task in SECOND dataset, our method achieved mIoU scores of 47.51\%, surpassing the second CS-MAE by 3 percentage points. Our pretrain code, checkpoints, and HR-Pairs dataset can be found in https://github.com/CVEO/MSSDF.
A Joint Representation Using Continuous and Discrete Features for Cardiovascular Diseases Risk Prediction on Chest CT Scans
Oct 24, 2024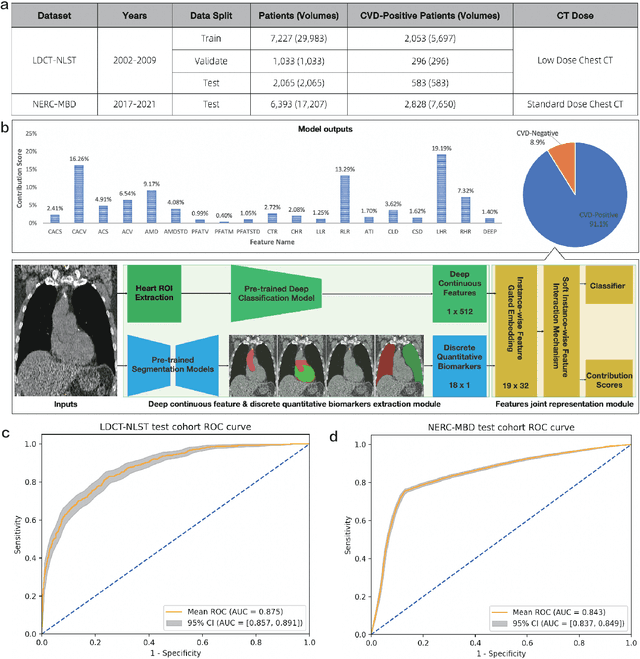
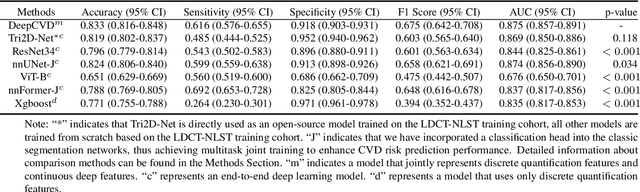
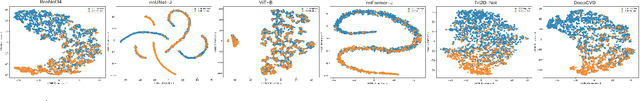
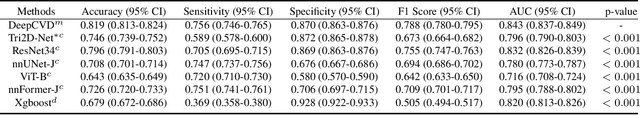
Abstract:Cardiovascular diseases (CVD) remain a leading health concern and contribute significantly to global mortality rates. While clinical advancements have led to a decline in CVD mortality, accurately identifying individuals who could benefit from preventive interventions remains an unsolved challenge in preventive cardiology. Current CVD risk prediction models, recommended by guidelines, are based on limited traditional risk factors or use CT imaging to acquire quantitative biomarkers, and still have limitations in predictive accuracy and applicability. On the other hand, end-to-end trained CVD risk prediction methods leveraging deep learning on CT images often fail to provide transparent and explainable decision grounds for assisting physicians. In this work, we proposed a novel joint representation that integrates discrete quantitative biomarkers and continuous deep features extracted from chest CT scans. Our approach initiated with a deep CVD risk classification model by capturing comprehensive continuous deep learning features while jointly obtaining currently clinical-established quantitative biomarkers via segmentation models. In the feature joint representation stage, we use an instance-wise feature-gated mechanism to align the continuous and discrete features, followed by a soft instance-wise feature interaction mechanism fostering independent and effective feature interaction for the final CVD risk prediction. Our method substantially improves CVD risk predictive performance and offers individual contribution analysis of each biomarker, which is important in assisting physicians' decision-making processes. We validated our method on a public chest low-dose CT dataset and a private external chest standard-dose CT patient cohort of 17,207 CT volumes from 6,393 unique subjects, and demonstrated superior predictive performance, achieving AUCs of 0.875 and 0.843, respectively.
Rapid and Accurate Diagnosis of Acute Aortic Syndrome using Non-contrast CT: A Large-scale, Retrospective, Multi-center and AI-based Study
Jun 25, 2024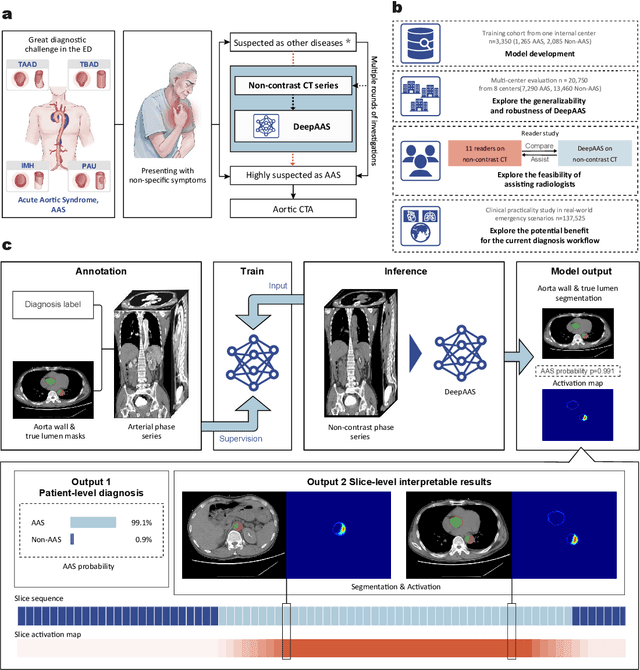
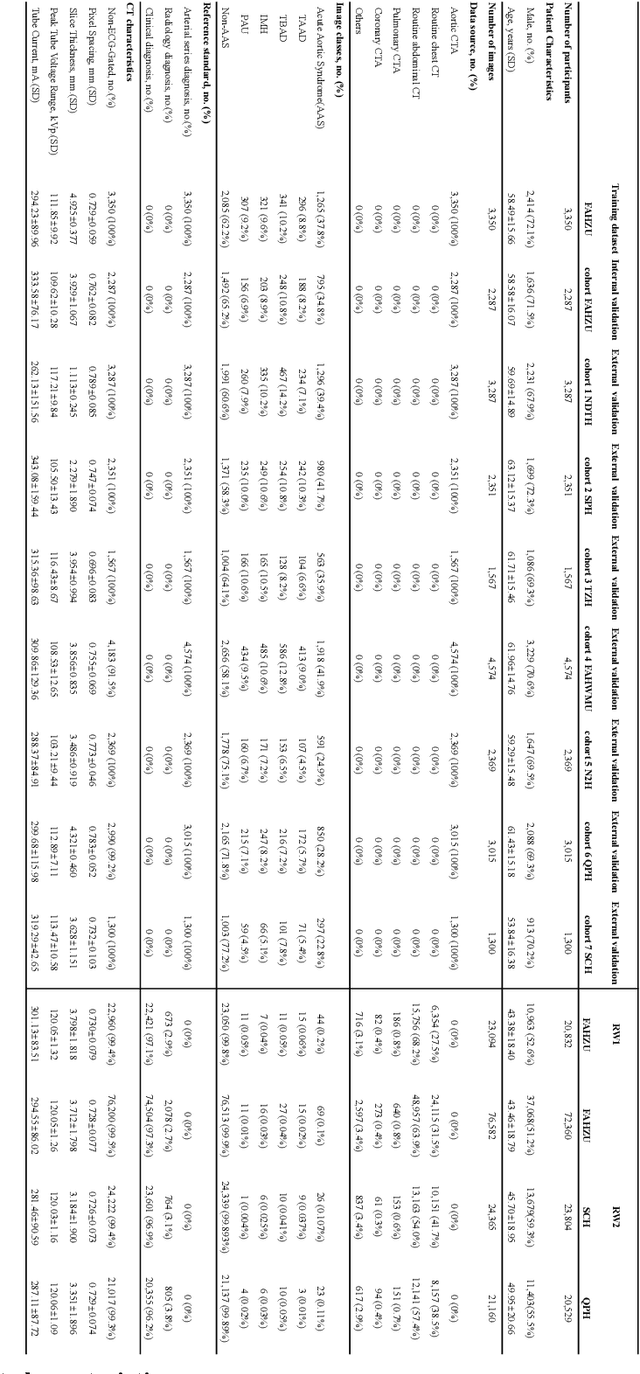
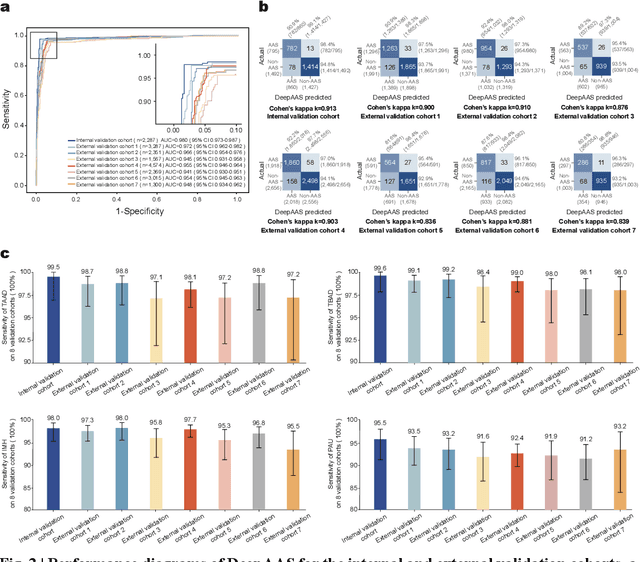
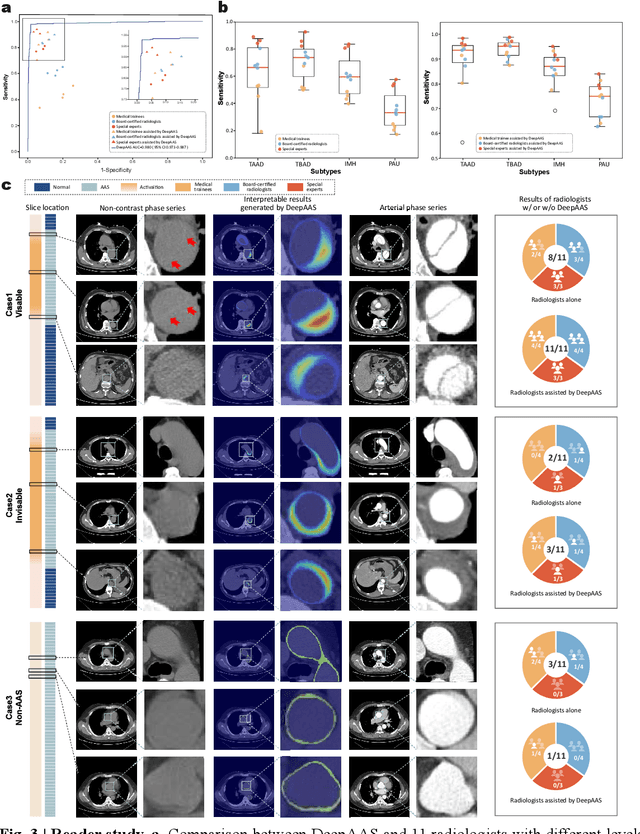
Abstract:Chest pain symptoms are highly prevalent in emergency departments (EDs), where acute aortic syndrome (AAS) is a catastrophic cardiovascular emergency with a high fatality rate, especially when timely and accurate treatment is not administered. However, current triage practices in the ED can cause up to approximately half of patients with AAS to have an initially missed diagnosis or be misdiagnosed as having other acute chest pain conditions. Subsequently, these AAS patients will undergo clinically inaccurate or suboptimal differential diagnosis. Fortunately, even under these suboptimal protocols, nearly all these patients underwent non-contrast CT covering the aorta anatomy at the early stage of differential diagnosis. In this study, we developed an artificial intelligence model (DeepAAS) using non-contrast CT, which is highly accurate for identifying AAS and provides interpretable results to assist in clinical decision-making. Performance was assessed in two major phases: a multi-center retrospective study (n = 20,750) and an exploration in real-world emergency scenarios (n = 137,525). In the multi-center cohort, DeepAAS achieved a mean area under the receiver operating characteristic curve of 0.958 (95% CI 0.950-0.967). In the real-world cohort, DeepAAS detected 109 AAS patients with misguided initial suspicion, achieving 92.6% (95% CI 76.2%-97.5%) in mean sensitivity and 99.2% (95% CI 99.1%-99.3%) in mean specificity. Our AI model performed well on non-contrast CT at all applicable early stages of differential diagnosis workflows, effectively reduced the overall missed diagnosis and misdiagnosis rate from 48.8% to 4.8% and shortened the diagnosis time for patients with misguided initial suspicion from an average of 681.8 (74-11,820) mins to 68.5 (23-195) mins. DeepAAS could effectively fill the gap in the current clinical workflow without requiring additional tests.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge