Taeyoon Son
Normalized Blood Flow Index in Optical Coherence Tomography Angiography Provides a Sensitive Biomarker of Early Diabetic Retinopathy
Dec 22, 2022Abstract:Purpose: To evaluate the sensitivity of normalized blood flow index (NBFI) for detecting early diabetic retinopathy (DR). Methods: Optical coherence tomography angiography (OCTA) images of 30 eyes from 20 healthy controls, 21 eyes of diabetic patients with no DR (NoDR) and 26 eyes from 22 patients with mild non-proliferative DR (NPDR) were analyzed in this study. The OCTA images were centered on the fovea and covered a 6 mm x 6 mm area. Enface projections of the superficial vascular plexus (SVP) and the deep capillary plexus (DCP) were obtained for the quantitative OCTA feature analysis. Three quantitative OCTA features were examined: blood vessel density (BVD), blood flow flux (BFF), and normalized blood flow index (NBFI). Each feature was calculated from both the SVP and DCP and their sensitivity to distinguish the three cohorts of the study were evaluated. Results: The only quantitative feature that was capable of distinguishing between all three cohorts was NBFI in the DCP image. Comparative study revealed that both BVD and BFF were able to distinguish the controls from NoDR and mild NPDR. However, neither BVD nor BFF was sensitive enough to separate NoDR from the healthy controls. Conclusion: The NBFI has been demonstrated as a sensitive biomarker of early DR, revealing retinal blood flow abnormality better than traditional BVD and BFF. The NBFI in the DCP was verified as the most sensitive biomarker, supporting that diabetes affects the DCP earlier than SVP in DR.
Functional Optical Coherence Tomography for Intrinsic Signal Optoretinography: Recent Developments and Deployment Challenges
Feb 18, 2022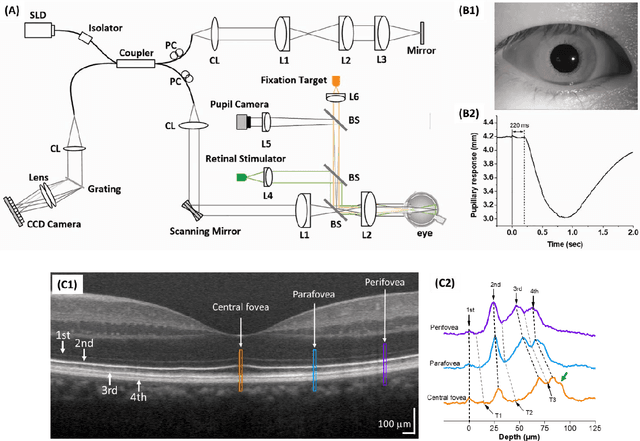
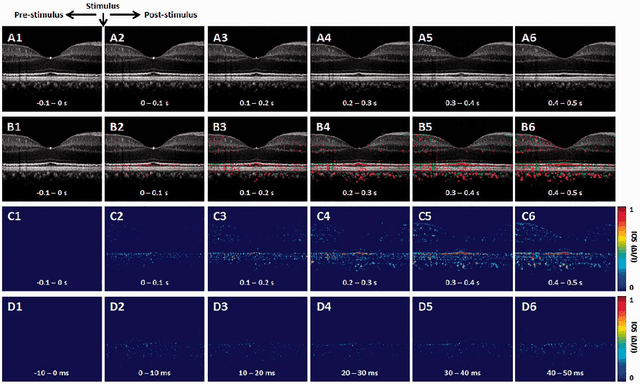


Abstract:Intrinsic optical signal (IOS) imaging of the retina, also termed as optoretinography (ORG), promises a noninvasive method for objective assessment of retinal function. By providing unparalleled capability to differentiate individual layers of the retina, functional optical coherence tomography (OCT) has been actively investigated for intrinsic signal ORG measurements. However, clinical deployment of functional OCT for quantitative ORG is still challenging due to the lack of a standardized imaging protocol and the complication of IOS sources and mechanisms. This article aims to summarize recent developments of functional OCT for ORG measurement, OCT intensity- and phase-based IOS processing. Technical challenges and perspectives of quantitative IOS analysis and ORG interpretations are discussed.
ADC-Net: An Open-Source Deep Learning Network for Automated Dispersion Compensation in Optical Coherence Tomography
Jan 29, 2022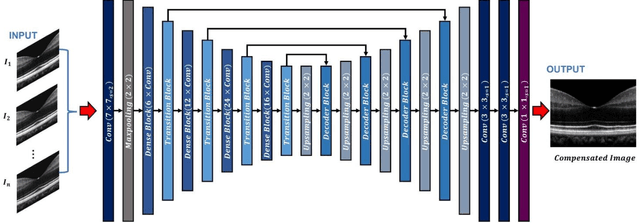
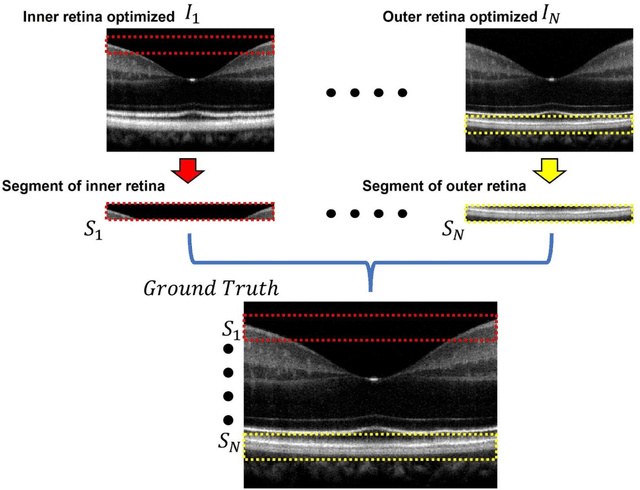
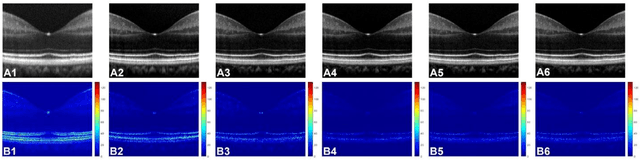
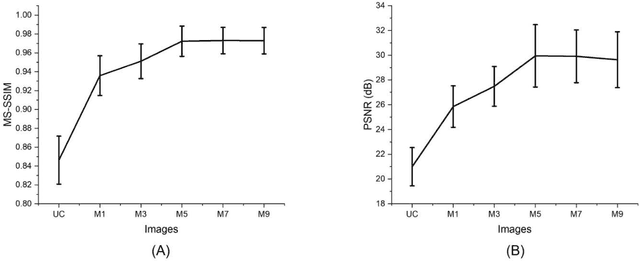
Abstract:Chromatic dispersion is a common problem to degrade the system resolution in optical coherence tomography (OCT). This study is to develop a deep learning network for automated dispersion compensation (ADC-Net) in OCT. The ADC-Net is based on a redesigned UNet architecture which employs an encoder-decoder pipeline. The input section encompasses partially compensated OCT B-scans with individual retinal layers optimized. Corresponding output is a fully compensated OCT B-scans with all retinal layers optimized. Two numeric parameters, i.e., peak signal to noise ratio (PSNR) and structural similarity index metric computed at multiple scales (MS-SSIM), were used for objective assessment of the ADC-Net performance. Comparative analysis of training models, including single, three, five, seven and nine input channels were implemented. The five-input channels implementation was observed as the optimal mode for ADC-Net training to achieve robust dispersion compensation in OCT
Depth-resolved vascular profile features for artery-vein classification in OCT and OCT angiography of human retina
Dec 14, 2021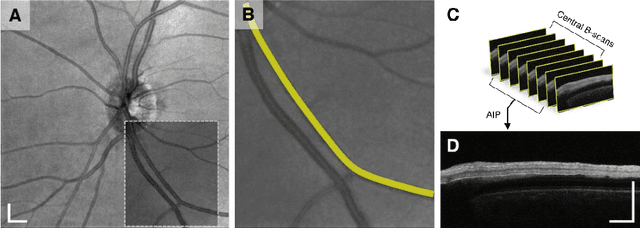
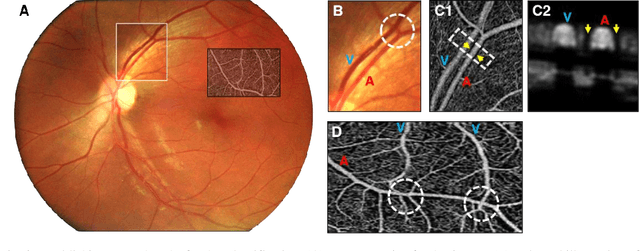
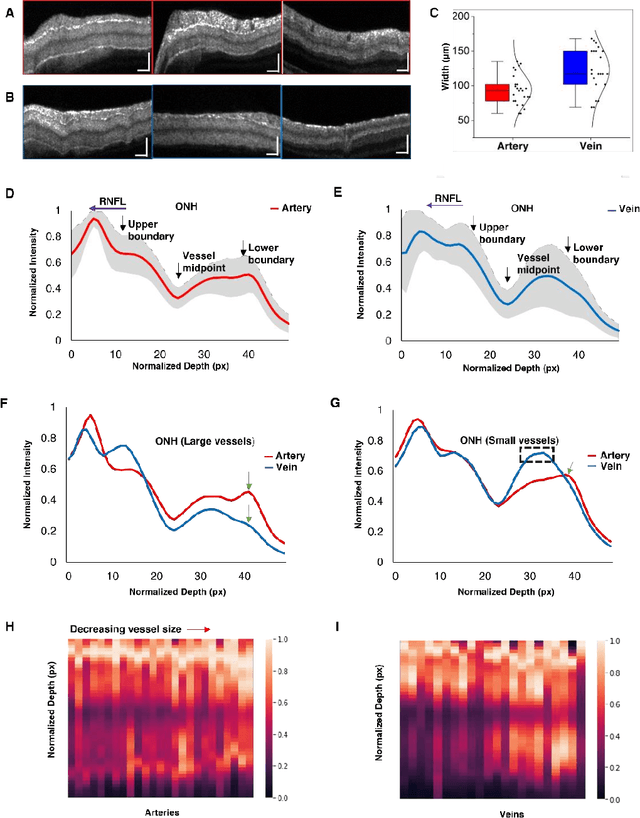
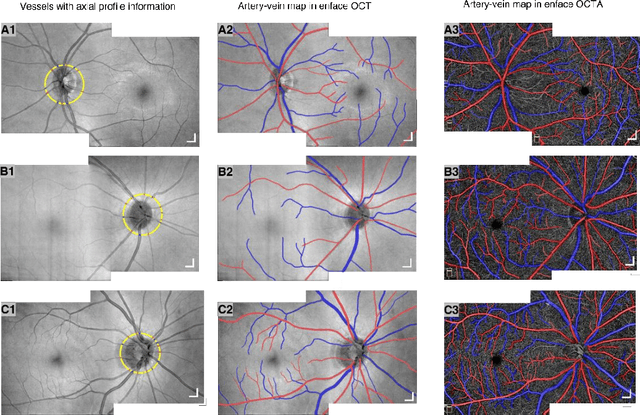
Abstract:This study is to characterize reflectance profiles of retinal blood vessels in optical coherence tomography (OCT), and to validate these vascular features to guide artery-vein classification in OCT angiography (OCTA) of human retina. Depth-resolved OCT reveals unique features of retinal arteries and veins. Retinal arteries show hyper-reflective boundaries at both upper (inner side towards the vitreous) and lower (outer side towards the choroid) walls. In contrary, retinal veins reveal hyper-reflectivity at the upper boundary only. Uniform lumen intensity was observed in both small and large arteries. However, the vein lumen intensity was dependent on the vessel size. Small veins exhibit a hyper-reflective zone at the bottom half of the lumen, while large veins show a hypo-reflective zone at the bottom half of the lumen
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge