Sung Jik Cha
Step-Calibrated Diffusion for Biomedical Optical Image Restoration
Mar 26, 2024



Abstract:High-quality, high-resolution medical imaging is essential for clinical care. Raman-based biomedical optical imaging uses non-ionizing infrared radiation to evaluate human tissues in real time and is used for early cancer detection, brain tumor diagnosis, and intraoperative tissue analysis. Unfortunately, optical imaging is vulnerable to image degradation due to laser scattering and absorption, which can result in diagnostic errors and misguided treatment. Restoration of optical images is a challenging computer vision task because the sources of image degradation are multi-factorial, stochastic, and tissue-dependent, preventing a straightforward method to obtain paired low-quality/high-quality data. Here, we present Restorative Step-Calibrated Diffusion (RSCD), an unpaired image restoration method that views the image restoration problem as completing the finishing steps of a diffusion-based image generation task. RSCD uses a step calibrator model to dynamically determine the severity of image degradation and the number of steps required to complete the reverse diffusion process for image restoration. RSCD outperforms other widely used unpaired image restoration methods on both image quality and perceptual evaluation metrics for restoring optical images. Medical imaging experts consistently prefer images restored using RSCD in blinded comparison experiments and report minimal to no hallucinations. Finally, we show that RSCD improves performance on downstream clinical imaging tasks, including automated brain tumor diagnosis and deep tissue imaging. Our code is available at https://github.com/MLNeurosurg/restorative_step-calibrated_diffusion.
Contrastive Representation Learning for Rapid Intraoperative Diagnosis of Skull Base Tumors Imaged Using Stimulated Raman Histology
Aug 08, 2021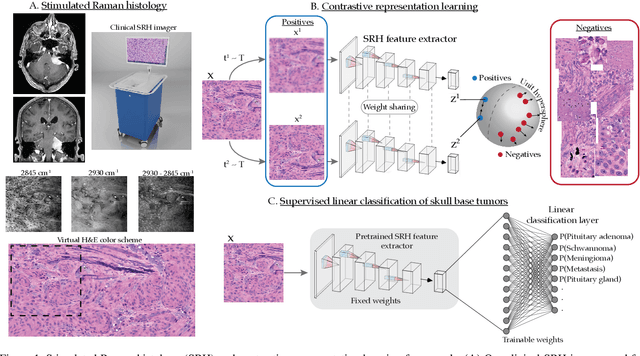
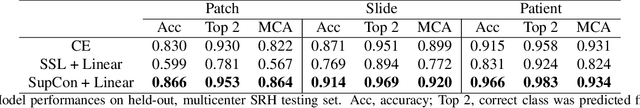
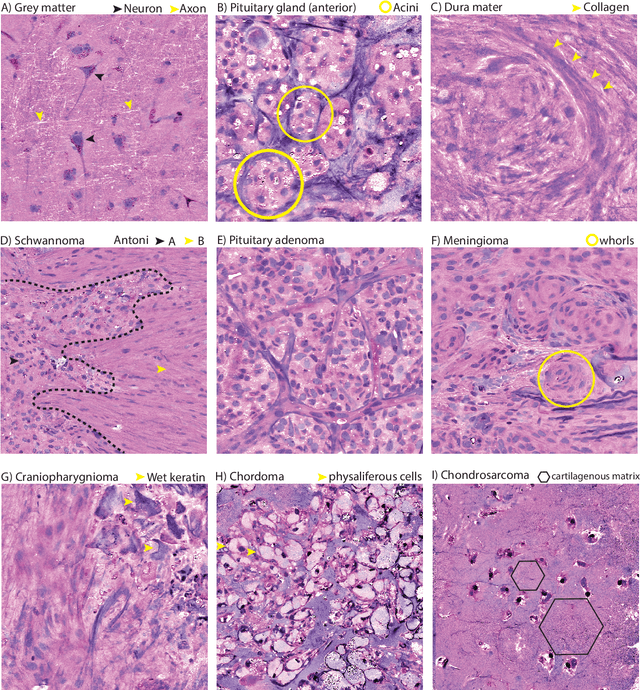
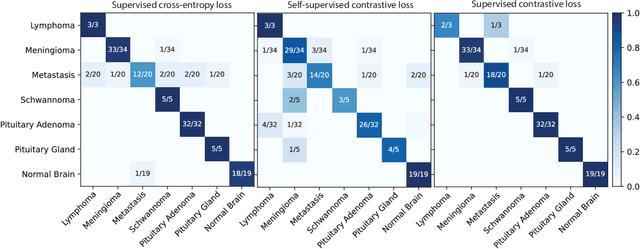
Abstract:Background: Accurate diagnosis of skull base tumors is essential for providing personalized surgical treatment strategies. Intraoperative diagnosis can be challenging due to tumor diversity and lack of intraoperative pathology resources. Objective: To develop an independent and parallel intraoperative pathology workflow that can provide rapid and accurate skull base tumor diagnoses using label-free optical imaging and artificial intelligence (AI). Method: We used a fiber laser-based, label-free, non-consumptive, high-resolution microscopy method ($<$ 60 sec per 1 $\times$ 1 mm$^\text{2}$), called stimulated Raman histology (SRH), to image a consecutive, multicenter cohort of skull base tumor patients. SRH images were then used to train a convolutional neural network (CNN) model using three representation learning strategies: cross-entropy, self-supervised contrastive learning, and supervised contrastive learning. Our trained CNN models were tested on a held-out, multicenter SRH dataset. Results: SRH was able to image the diagnostic features of both benign and malignant skull base tumors. Of the three representation learning strategies, supervised contrastive learning most effectively learned the distinctive and diagnostic SRH image features for each of the skull base tumor types. In our multicenter testing set, cross-entropy achieved an overall diagnostic accuracy of 91.5%, self-supervised contrastive learning 83.9%, and supervised contrastive learning 96.6%. Our trained model was able to identify tumor-normal margins and detect regions of microscopic tumor infiltration in whole-slide SRH images. Conclusion: SRH with AI models trained using contrastive representation learning can provide rapid and accurate intraoperative diagnosis of skull base tumors.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge