Miriam Mikhelson
Development and Evaluation of Three Chatbots for Postpartum Mood and Anxiety Disorders
Aug 14, 2023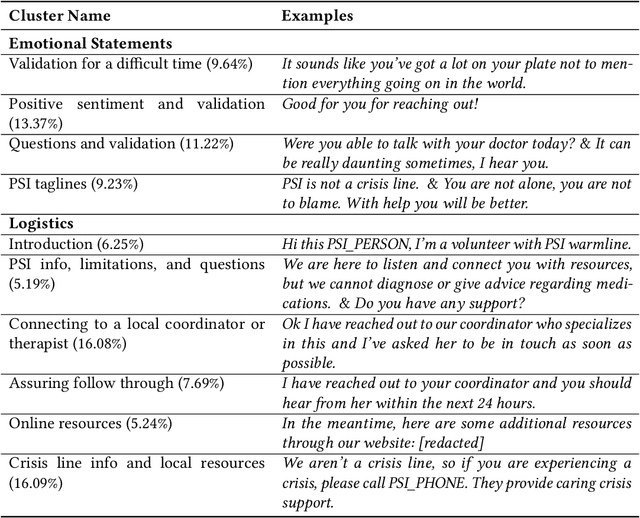
Abstract:In collaboration with Postpartum Support International (PSI), a non-profit organization dedicated to supporting caregivers with postpartum mood and anxiety disorders, we developed three chatbots to provide context-specific empathetic support to postpartum caregivers, leveraging both rule-based and generative models. We present and evaluate the performance of our chatbots using both machine-based metrics and human-based questionnaires. Overall, our rule-based model achieves the best performance, with outputs that are close to ground truth reference and contain the highest levels of empathy. Human users prefer the rule-based chatbot over the generative chatbot for its context-specific and human-like replies. Our generative chatbot also produced empathetic responses and was described by human users as engaging. However, limitations in the training dataset often result in confusing or nonsensical responses. We conclude by discussing practical benefits of rule-based vs. generative models for supporting individuals with mental health challenges. In light of the recent surge of ChatGPT and BARD, we also discuss the possibilities and pitfalls of large language models for digital mental healthcare.
Understanding Postpartum Parents' Experiences via Two Digital Platforms
Dec 22, 2022



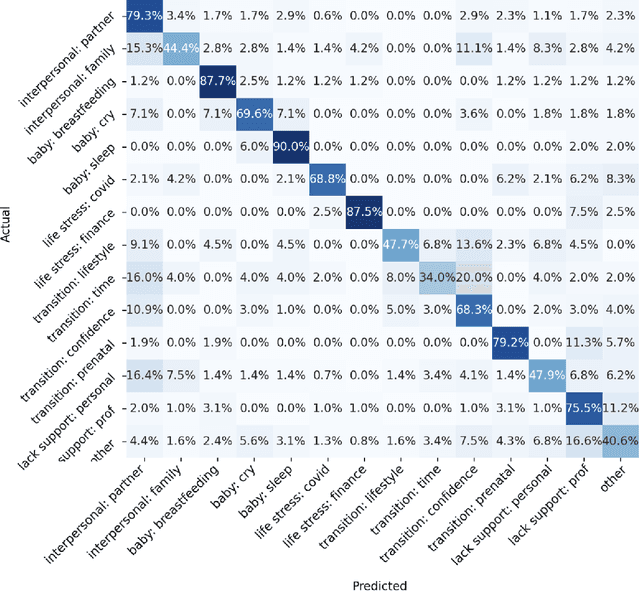
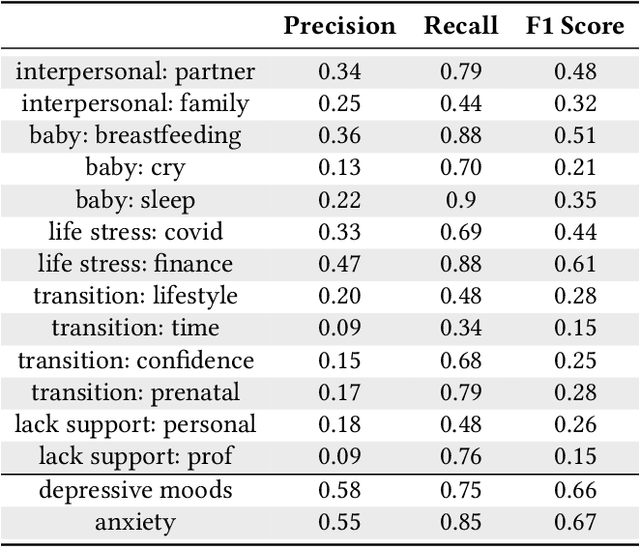
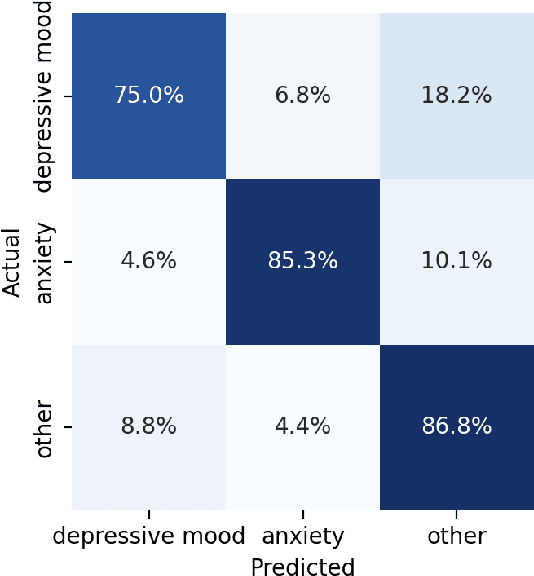
Abstract:Digital platforms, including online forums and helplines, have emerged as avenues of support for caregivers suffering from postpartum mental health distress. Understanding support seekers' experiences as shared on these platforms could provide crucial insight into caregivers' needs during this vulnerable time. In the current work, we provide a descriptive analysis of the concerns, psychological states, and motivations shared by healthy and distressed postpartum support seekers on two digital platforms, a one-on-one digital helpline and a publicly available online forum. Using a combination of human annotations, dictionary models and unsupervised techniques, we find stark differences between the experiences of distressed and healthy mothers. Distressed mothers described interpersonal problems and a lack of support, with 8.60% - 14.56% reporting severe symptoms including suicidal ideation. In contrast, the majority of healthy mothers described childcare issues, such as questions about breastfeeding or sleeping, and reported no severe mental health concerns. Across the two digital platforms, we found that distressed mothers shared similar content. However, the patterns of speech and affect shared by distressed mothers differed between the helpline vs. the online forum, suggesting the design of these platforms may shape meaningful measures of their support-seeking experiences. Our results provide new insight into the experiences of caregivers suffering from postpartum mental health distress. We conclude by discussing methodological considerations for understanding content shared by support seekers and design considerations for the next generation of support tools for postpartum parents.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge