Maximilian Dietrich
Department of Anesthesiology, Heidelberg University Hospital, Heidelberg, Germany
New spectral imaging biomarkers for sepsis and mortality in intensive care
Aug 19, 2024Abstract:With sepsis remaining a leading cause of mortality, early identification of septic patients and those at high risk of death is a challenge of high socioeconomic importance. The driving hypothesis of this study was that hyperspectral imaging (HSI) could provide novel biomarkers for sepsis diagnosis and treatment management due to its potential to monitor microcirculatory alterations. We conducted a comprehensive study involving HSI data of the palm and fingers from more than 480 patients on the day of their intensive care unit (ICU) admission. The findings demonstrate that HSI measurements can predict sepsis with an area under the receiver operating characteristic curve (AUROC) of 0.80 (95 % confidence interval (CI) [0.76; 0.84]) and mortality with an AUROC of 0.72 (95 % CI [0.65; 0.79]). The predictive performance improves substantially when additional clinical data is incorporated, leading to an AUROC of up to 0.94 (95 % CI [0.92; 0.96]) for sepsis and 0.84 (95 % CI [0.78; 0.89]) for mortality. We conclude that HSI presents novel imaging biomarkers for the rapid, non-invasive prediction of sepsis and mortality, suggesting its potential as an important modality for guiding diagnosis and treatment.
Machine learning-based analysis of hyperspectral images for automated sepsis diagnosis
Jun 15, 2021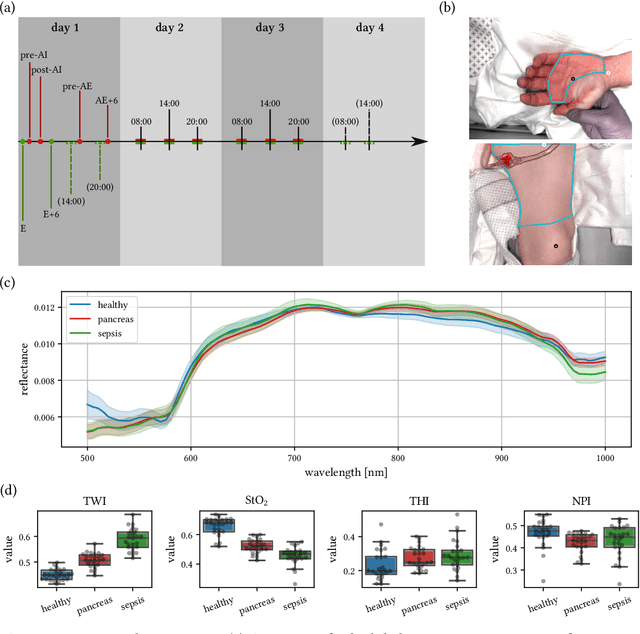
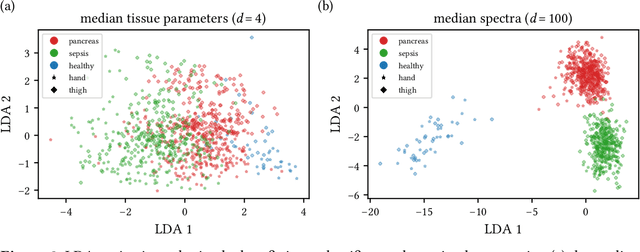
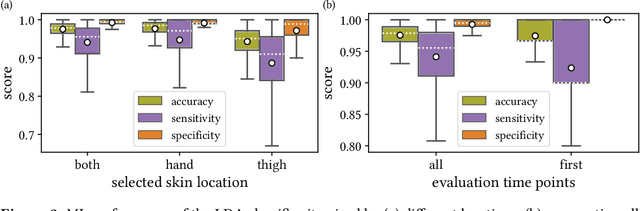
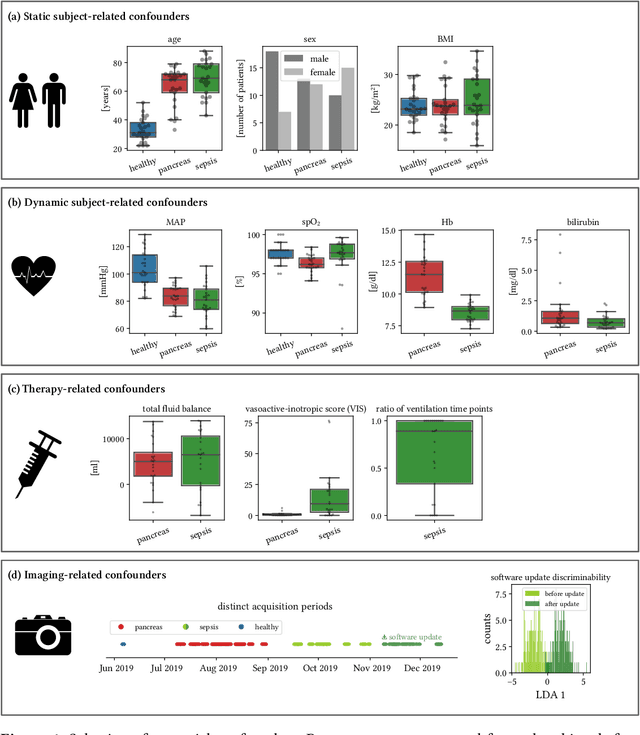
Abstract:Sepsis is a leading cause of mortality and critical illness worldwide. While robust biomarkers for early diagnosis are still missing, recent work indicates that hyperspectral imaging (HSI) has the potential to overcome this bottleneck by monitoring microcirculatory alterations. Automated machine learning-based diagnosis of sepsis based on HSI data, however, has not been explored to date. Given this gap in the literature, we leveraged an existing data set to (1) investigate whether HSI-based automated diagnosis of sepsis is possible and (2) put forth a list of possible confounders relevant for HSI-based tissue classification. While we were able to classify sepsis with an accuracy of over $98\,\%$ using the existing data, our research also revealed several subject-, therapy- and imaging-related confounders that may lead to an overestimation of algorithm performance when not balanced across the patient groups. We conclude that further prospective studies, carefully designed with respect to these confounders, are necessary to confirm the preliminary results obtained in this study.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge