Jukka Hirvasniemi
Early detection of knee osteoarthritis using deep learning on knee magnetic resonance images
Sep 02, 2022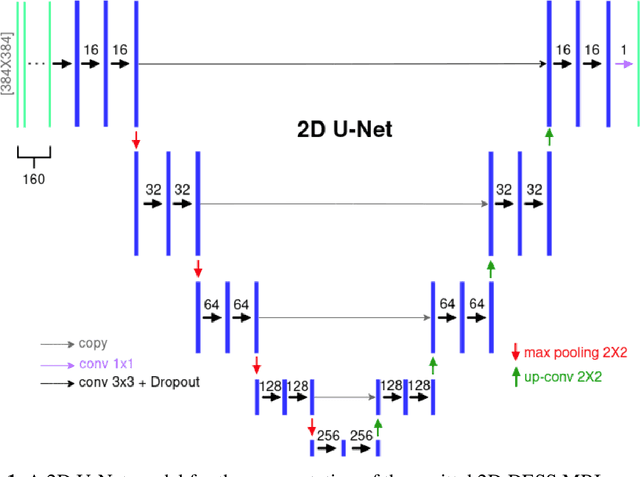

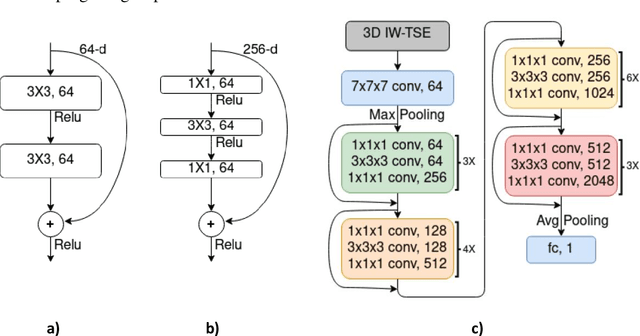
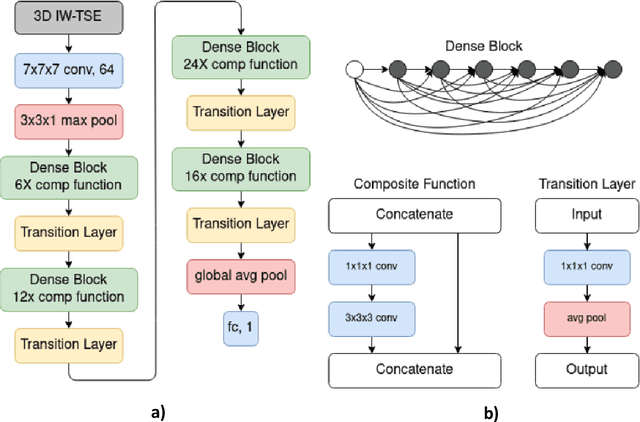
Abstract:The aim of this study was to investigate the influence of MRI and patient data on the prediction of knee osteoarthritis (OA) incidence using different deep learning architectures. Knee OA incidence within 24 months was predicted using the intermediate-weighted turbo spin-echo (IW-TSE) sequence of 593 patients from the Osteoarthritis Initiative. To extract a region of interest containing the knee joint from the IW-TSE sequence, a U-Net model was trained and used to segment bone on a dual echo steady state (DESS) sequence. Subsequently, IW-TSE and DESS sequences were registered and the DESS segmentations were transformed to the corresponding IW-TSE scans. The performance of MRI-based features in the prediction of knee OA incidence was tested using three different deep learning architectures: a residual network (ResNet), a densely connected convolutional network (DenseNet), and a convolutional variational autoencoder (CVAE). To evaluate the predictive performance of MRI-based features alone, the outputs of ResNet, DenseNet, and CVAE were coupled with patient data (i.e., age, gender, BMI) and used as input to a Logistic Regression (LR) Classifier. Knee OA was defined based on visual MRI and X-ray-based OA features. The ResNet and DenseNet showed similar results, with both methods having the area under the receiver operating characteristic curve (AUC) values up to 0.6269. The best performing OA detection model was CVAE with an AUC of 0.6699 when combined with patient data and an AUC of 0.6689 when used alone as input to the LR classifier. The results showed that three deep learning algorithms have similar metrics when using IW-TSE MRIs and their performance increased with the inclusion of patient data, which shows the strong influence of variables such as age, gender, and BMI on the detection of knee OA.
Adaptive Segmentation of Knee Radiographs for Selecting the Optimal ROI in Texture Analysis
Aug 21, 2019



Abstract:The purposes of this study were to investigate: 1) the effect of placement of region-of-interest (ROI) for texture analysis of subchondral bone in knee radiographs, and 2) the ability of several texture descriptors to distinguish between the knees with and without radiographic osteoarthritis (OA). Bilateral posterior-anterior knee radiographs were analyzed from the baseline of OAI and MOST datasets. A fully automatic method to locate the most informative region from subchondral bone using adaptive segmentation was developed. We used an oversegmentation strategy for partitioning knee images into the compact regions that follow natural texture boundaries. LBP, Fractal Dimension (FD), Haralick features, Shannon entropy, and HOG methods were computed within the standard ROI and within the proposed adaptive ROIs. Subsequently, we built logistic regression models to identify and compare the performances of each texture descriptor and each ROI placement method using 5-fold cross validation setting. Importantly, we also investigated the generalizability of our approach by training the models on OAI and testing them on MOST dataset.We used area under the receiver operating characteristic (ROC) curve (AUC) and average precision (AP) obtained from the precision-recall (PR) curve to compare the results. We found that the adaptive ROI improves the classification performance (OA vs. non-OA) over the commonly used standard ROI (up to 9% percent increase in AUC). We also observed that, from all texture parameters, LBP yielded the best performance in all settings with the best AUC of 0.840 [0.825, 0.852] and associated AP of 0.804 [0.786, 0.820]. Compared to the current state-of-the-art approaches, our results suggest that the proposed adaptive ROI approach in texture analysis of subchondral bone can increase the diagnostic performance for detecting the presence of radiographic OA.
Bone Texture Analysis for Prediction of Incident Radio-graphic Hip Osteoarthritis Using Machine Learning: Data from the Cohort Hip and Cohort Knee (CHECK) study
Feb 13, 2019



Abstract:Our aim was to assess the ability of radiography-based bone texture parameters in proximal femur and acetabulum to predict incident radiographic hip osteoarthritis (rHOA) over a 10 years period. Pelvic radiographs from CHECK (Cohort Hip and Cohort Knee) at baseline (987 hips) were analyzed for bone texture using fractal signature analysis in proximal femur and acetabulum. Elastic net (machine learning) was used to predict the incidence of rHOA (Kellgren-Lawrence grade (KL) > 1 or total hip replacement (THR)), joint space narrowing score (JSN, range 0-3), and osteophyte score (OST, range 0-3) after 10 years. Performance of prediction models was assessed using the area under the receiver operating characteristic curve (ROC AUC). Of the 987 hips without rHOA at baseline, 435 (44%) had rHOA at 10-year follow-up. Of the 667 hips with JSN grade 0 at baseline, 471 (71%) had JSN grade > 0 at 10-year follow-up. Of the 613 hips with OST grade 0 at baseline, 526 (86%) had OST grade > 0 at 10-year follow-up. AUCs for the models including age, gender, and body mass index to predict incident rHOA, JSN, and OST were 0.59, 0.54, and 0.51, respectively. The inclusion of bone texture parameters in the models improved the prediction of incident rHOA (ROC AUC 0.66 and 0.71 when baseline KL was also included in the model) and JSN (ROC AUC 0.62), but not incident OST (ROC AUC 0.53). Bone texture analysis provides additional information for predicting incident rHOA or THR over 10 years.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge