Jefferson Chen
Fully Automated Volumetric Classification in CT Scans for Diagnosis and Analysis of Normal Pressure Hydrocephalus
Jan 25, 2019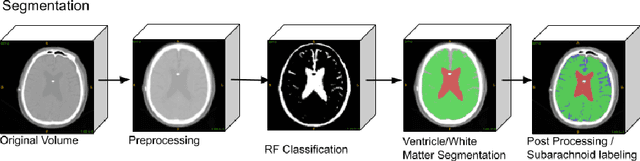
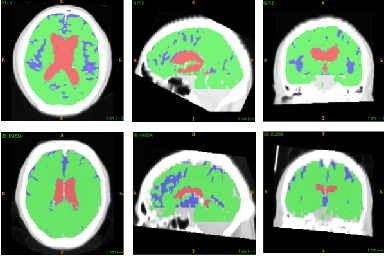
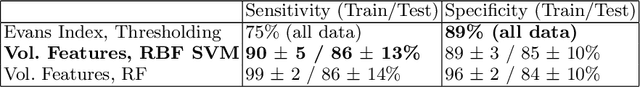
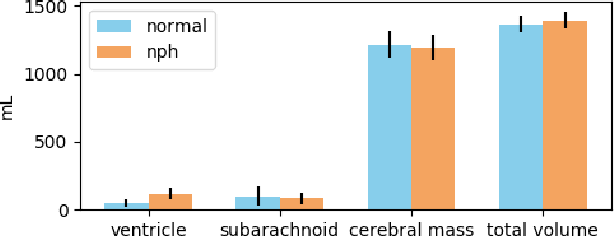
Abstract:Normal Pressure Hydrocephalus (NPH) is one of the few reversible forms of dementia. Due to their low cost and versatility, Computed Tomography (CT) scans have long been used as an aid to help diagnose intracerebral anomalies such as NPH. However, because CT imaging presents 2-dimensional slices of a 3-dimensional volume, recapitulating the ventricular space in 3-dimensions to facilitate the diagnosis of NPH poses numerous challenges such as head rotation and human error. As such, no well-defined and effective protocol currently exists for the analysis of CT scan-based ventricular, white matter and subarachnoid space volumes in the setting of NPH. The Evan's ratio, an approximation of the ratio of ventricle to brain volume using only one 2D slice of the scan, has been proposed but is not robust. Instead of manually measuring a 2-dimensional proxy for the ratio of ventricle volume to brain volume, this study proposes an automated method of calculating the brain volumes for better recognition of NPH from a radiological standpoint. The method first aligns the subject CT volume to a common space through an affine transformation, then uses a random forest classifier to mask relevant tissue types. A 3D morphological segmentation method is used to partition the brain volume, which in turn is used to train machine learning methods to classify the subjects into non-NPH vs. NPH based on volumetric information.
Brain Tumor Segmentation and Tractographic Feature Extraction from Structural MR Images for Overall Survival Prediction
Oct 10, 2018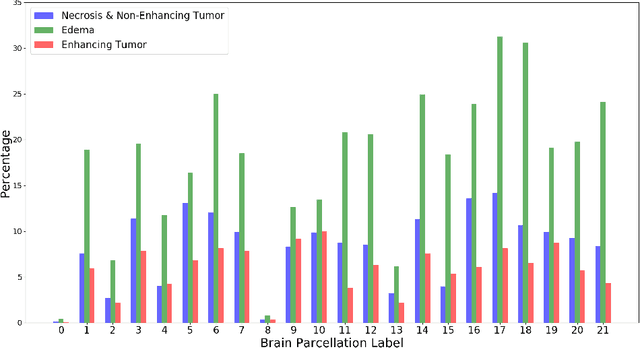
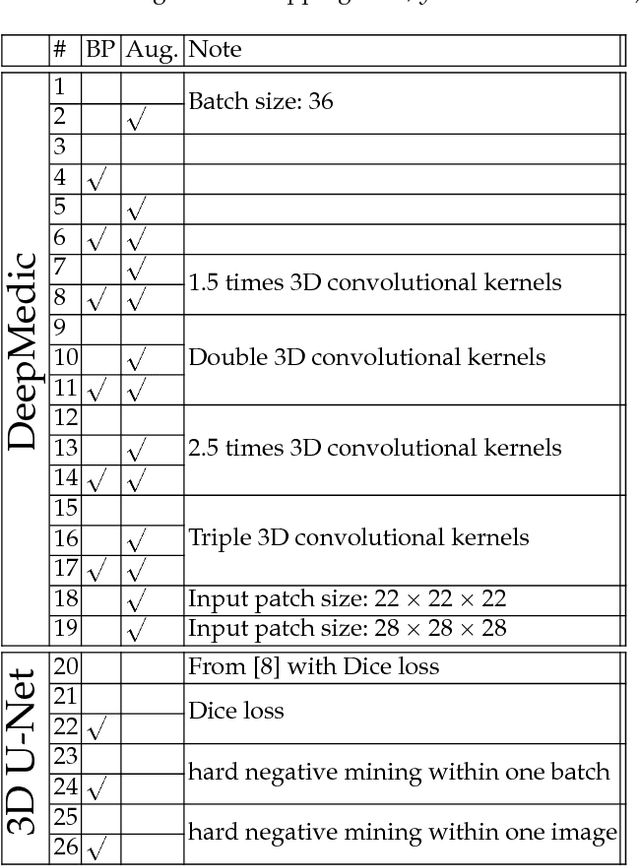
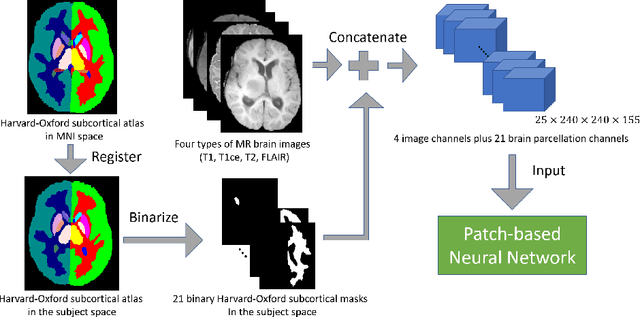

Abstract:This paper introduces a novel methodology to integrate human brain connectomics and parcellation for brain tumor segmentation and survival prediction. For segmentation, we utilize an existing brain parcellation atlas in the MNI152 1mm space and map this parcellation to each individual subject data. We use deep neural network architectures together with hard negative mining to achieve the final voxel level classification. For survival prediction, we present a new method for combining features from connectomics data, brain parcellation information, and the brain tumor mask. We leverage the average connectome information from the Human Connectome Project and map each subject brain volume onto this common connectome space. From this, we compute tractographic features that describe potential neural disruptions due to the brain tumor. These features are then used to predict the overall survival of the subjects. The main novelty in the proposed methods is the use of normalized brain parcellation data and tractography data from the human connectome project for analyzing MR images for segmentation and survival prediction. Experimental results are reported on the BraTS2018 data.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge