Jéssica A. Canazart
Automatic Diagnosis of the Short-Duration 12-Lead ECG using a Deep Neural Network: the CODE Study
Apr 02, 2019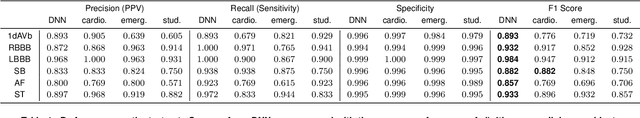
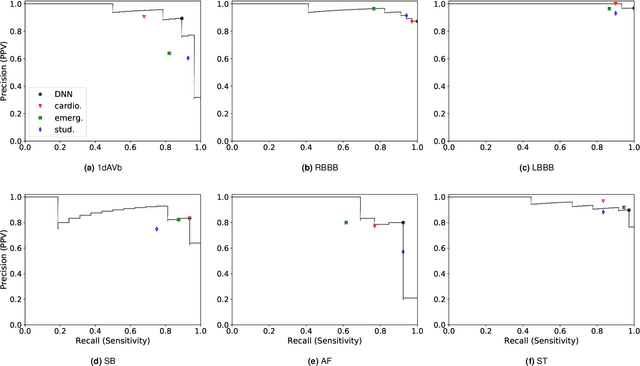
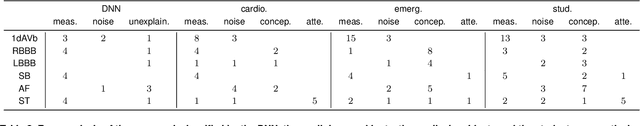
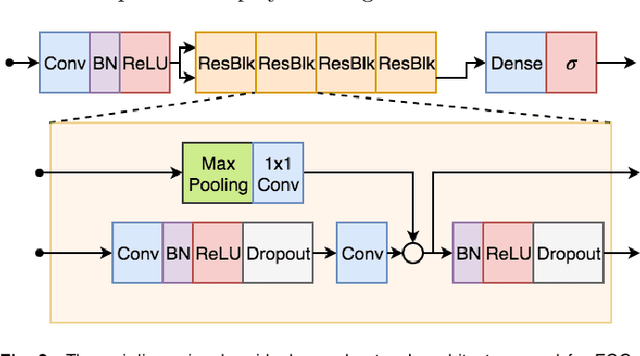
Abstract:We present a Deep Neural Network (DNN) model for predicting electrocardiogram (ECG) abnormalities in short-duration 12-lead ECG recordings. The analysis of the digital ECG obtained in a clinical setting can provide a full evaluation of the cardiac electrical activity and have not been studied in an end-to-end machine learning scenario. Using the database of the Telehealth Network of Minas Gerais, under the scope of the CODE (Clinical Outcomes in Digital Electrocardiology) study, we built a novel dataset with more than 2 million ECG tracings, orders of magnitude larger than those used in previous studies. Moreover, our dataset is more realistic, as it consists of 12-lead ECGs recorded during standard in-clinic exams. Using this data, we trained a residual neural network with 9 convolutional layers to map ECG signals with a duration of 7 to 10 seconds into 6 different classes of ECG abnormalities. High-performance measures were obtained for all ECG abnormalities, with F1 scores above $80\%$ and specificity indexes over $99\%$. We compare the performance with cardiology and emergency resident medical doctors as well as medical students and, considering the F1 score, the DNN matches or outperforms the medical residents and students for all abnormalities. These results indicate that end-to-end automatic ECG analysis based on DNNs, previously used only in a single-lead setup, generalizes well to the 12-lead ECG. This is an important result in that it takes this technology much closer to standard clinical practice.
Automatic Diagnosis of Short-Duration 12-Lead ECG using a Deep Convolutional Network
Nov 28, 2018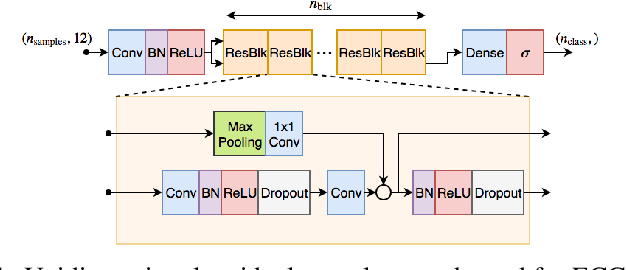
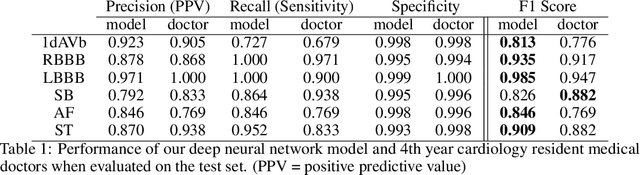
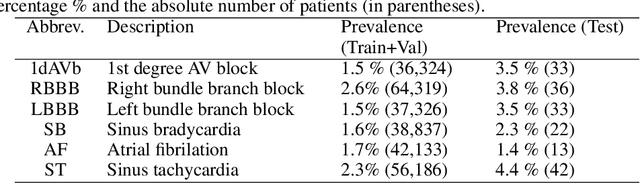
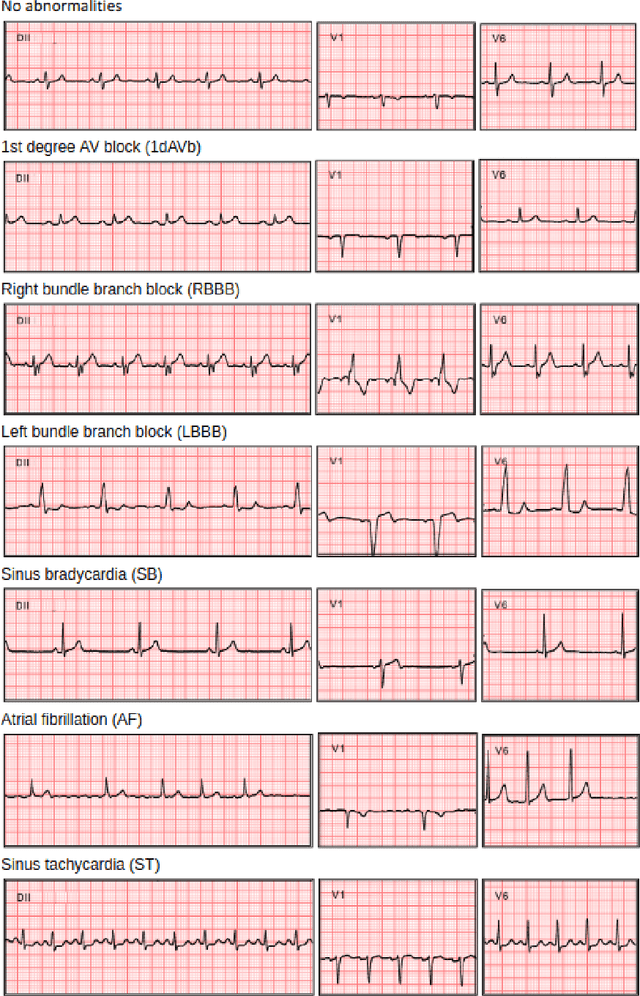
Abstract:We present a model for predicting electrocardiogram (ECG) abnormalities in short-duration 12-lead ECG signals which outperformed medical doctors on the 4th year of their cardiology residency. Such exams can provide a full evaluation of heart activity and have not been studied in previous end-to-end machine learning papers. Using the database of a large telehealth network, we built a novel dataset with more than 2 million ECG tracings, orders of magnitude larger than those used in previous studies. Moreover, our dataset is more realistic, as it consist of 12-lead ECGs recorded during standard in-clinics exams. Using this data, we trained a residual neural network with 9 convolutional layers to map 7 to 10 second ECG signals to 6 classes of ECG abnormalities. Future work should extend these results to cover a large range of ECG abnormalities, which could improve the accessibility of this diagnostic tool and avoid wrong diagnosis from medical doctors.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge