Greg Sorensen
Validation of a deep learning mammography model in a population with low screening rates
Nov 01, 2019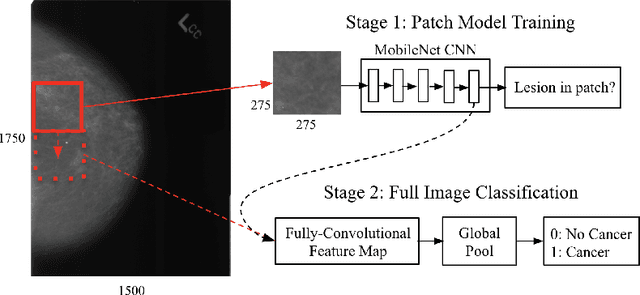
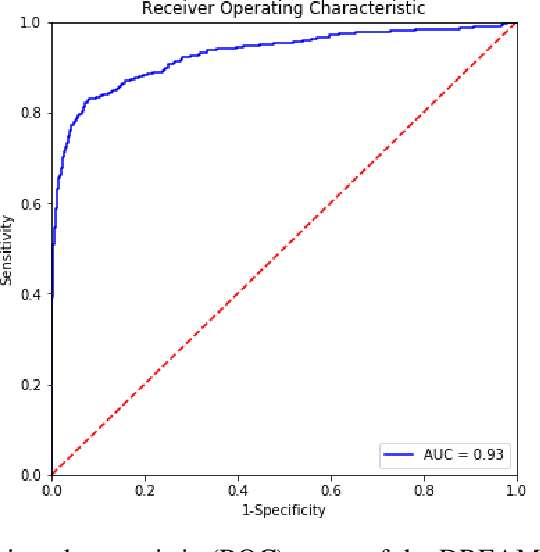
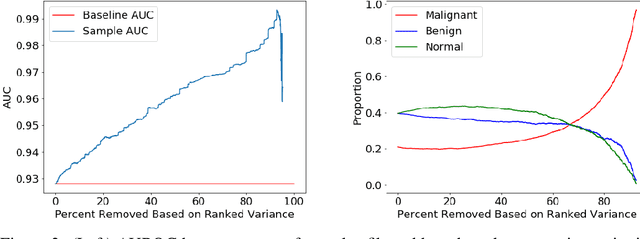
Abstract:A key promise of AI applications in healthcare is in increasing access to quality medical care in under-served populations and emerging markets. However, deep learning models are often only trained on data from advantaged populations that have the infrastructure and resources required for large-scale data collection. In this paper, we aim to empirically investigate the potential impact of such biases on breast cancer detection in mammograms. We specifically explore how a deep learning algorithm trained on screening mammograms from the US and UK generalizes to mammograms collected at a hospital in China, where screening is not widely implemented. For the evaluation, we use a top-scoring model developed for the Digital Mammography DREAM Challenge. Despite the change in institution and population composition, we find that the model generalizes well, exhibiting similar performance to that achieved in the DREAM Challenge, even when controlling for tumor size. We also illustrate a simple but effective method for filtering predictions based on model variance, which can be particularly useful for deployment in new settings. While there are many components in developing a clinically effective system, these results represent a promising step towards increasing access to life-saving screening mammography in populations where screening rates are currently low.
A Multi-Scale CNN and Curriculum Learning Strategy for Mammogram Classification
Jul 21, 2017



Abstract:Screening mammography is an important front-line tool for the early detection of breast cancer, and some 39 million exams are conducted each year in the United States alone. Here, we describe a multi-scale convolutional neural network (CNN) trained with a curriculum learning strategy that achieves high levels of accuracy in classifying mammograms. Specifically, we first train CNN-based patch classifiers on segmentation masks of lesions in mammograms, and then use the learned features to initialize a scanning-based model that renders a decision on the whole image, trained end-to-end on outcome data. We demonstrate that our approach effectively handles the "needle in a haystack" nature of full-image mammogram classification, achieving 0.92 AUROC on the DDSM dataset.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge