Dirk Fortmeier
Evaluation of Direct Haptic 4D Volume Rendering of Partially Segmented Data for Liver Puncture Simulation
May 19, 2017

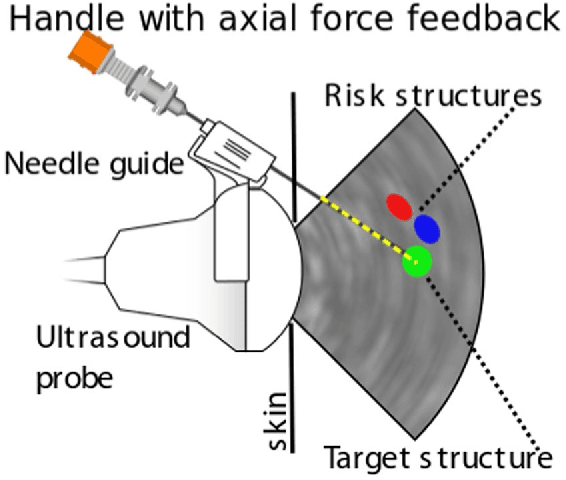

Abstract:This work presents an evaluation study using a force feedback evaluation framework for a novel direct needle force volume rendering concept in the context of liver puncture simulation. PTC/PTCD puncture interventions targeting the bile ducts have been selected to illustrate this concept. The haptic algorithms of the simulator system are based on (1) partially segmented patient image data and (2) a non-linear spring model effective at organ borders. The primary aim is to quantitatively evaluate force errors caused by our patient modeling approach, in comparison to haptic force output obtained from using gold-standard, completely manually-segmented data. The evaluation of the force algorithms compared to a force output from fully manually segmented gold-standard patient models, yields a low mean of 0.12 N root mean squared force error and up to 1.6 N for systematic maximum absolute errors. Force errors were evaluated on 31,222 preplanned test paths from 10 patients. Only twelve percent of the emitted forces along these paths were affected by errors. This is the first study evaluating haptic algorithms with deformable virtual patients in silico. We prove haptic rendering plausibility on a very high number of test paths. Important errors are below just noticeable differences for the hand-arm system.
* 15 pages, 16 figures, 1 tables, 11 equations, 39 references
Model-based Catheter Segmentation in MRI-images
May 18, 2017


Abstract:Accurate and reliable segmentation of catheters in MR-gui- ded interventions remains a challenge, and a step of critical importance in clinical workflows. In this work, under reasonable assumptions, me- chanical model based heuristics guide the segmentation process allows correct catheter identification rates greater than 98% (error 2.88 mm), and reduction in outliers to one-fourth compared to the state of the art. Given distal tips, searching towards the proximal ends of the catheters is guided by mechanical models that are estimated on a per-catheter basis. Their bending characteristics are used to constrain the image fea- ture based candidate points. The final catheter trajectories are hybrid sequences of individual points, each derived from model and image fea- tures. We evaluate the method on a database of 10 patient MRI scans including 101 manually segmented catheters. The mean errors were 1.40 mm and the median errors were 1.05 mm. The number of outliers devi- ating more than 2 mm from the gold standard is 7, and the number of outliers deviating more than 3 mm from the gold standard is just 2.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge