David J. Stone
Prediction of Blood Lactate Values in Critically Ill Patients: A Retrospective Multi-center Cohort Study
Jul 07, 2021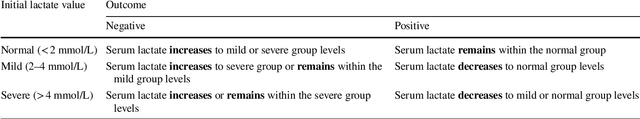
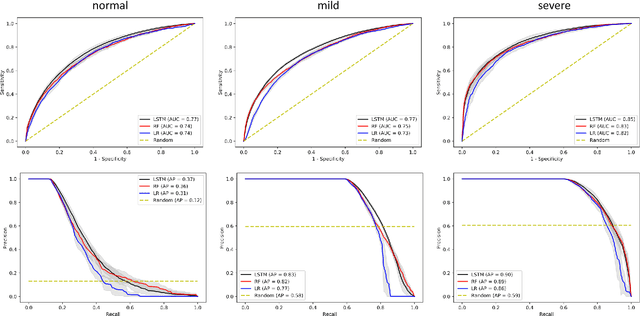
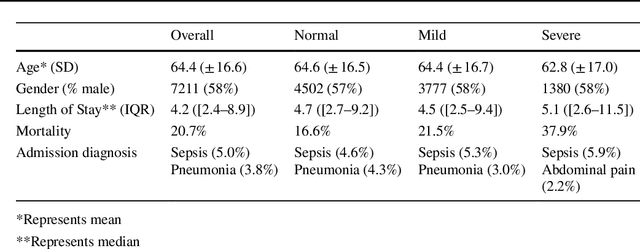
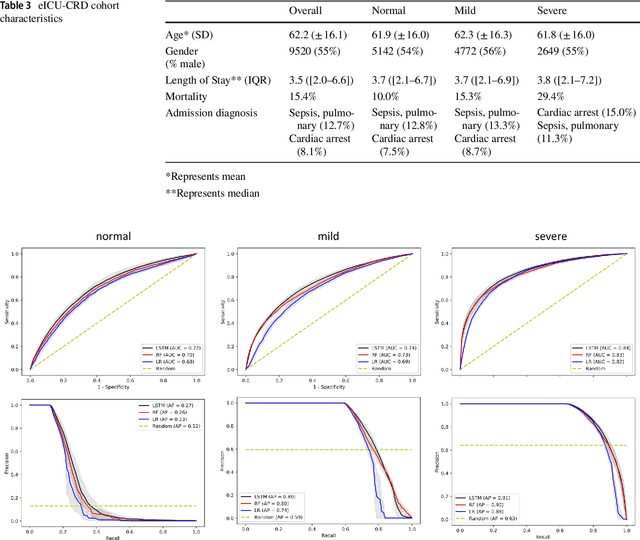
Abstract:Purpose. Elevations in initially obtained serum lactate levels are strong predictors of mortality in critically ill patients. Identifying patients whose serum lactate levels are more likely to increase can alert physicians to intensify care and guide them in the frequency of tending the blood test. We investigate whether machine learning models can predict subsequent serum lactate changes. Methods. We investigated serum lactate change prediction using the MIMIC-III and eICU-CRD datasets in internal as well as external validation of the eICU cohort on the MIMIC-III cohort. Three subgroups were defined based on the initial lactate levels: i) normal group (<2 mmol/L), ii) mild group (2-4 mmol/L), and iii) severe group (>4 mmol/L). Outcomes were defined based on increase or decrease of serum lactate levels between the groups. We also performed sensitivity analysis by defining the outcome as lactate change of >10% and furthermore investigated the influence of the time interval between subsequent lactate measurements on predictive performance. Results. The LSTM models were able to predict deterioration of serum lactate values of MIMIC-III patients with an AUC of 0.77 (95% CI 0.762-0.771) for the normal group, 0.77 (95% CI 0.768-0.772) for the mild group, and 0.85 (95% CI 0.840-0.851) for the severe group, with a slightly lower performance in the external validation. Conclusion. The LSTM demonstrated good discrimination of patients who had deterioration in serum lactate levels. Clinical studies are needed to evaluate whether utilization of a clinical decision support tool based on these results could positively impact decision-making and patient outcomes.
* 15 pages, 6 Appendices
Withholding aggressive treatments may not accelerate time to death among dying ICU patients
Aug 04, 2018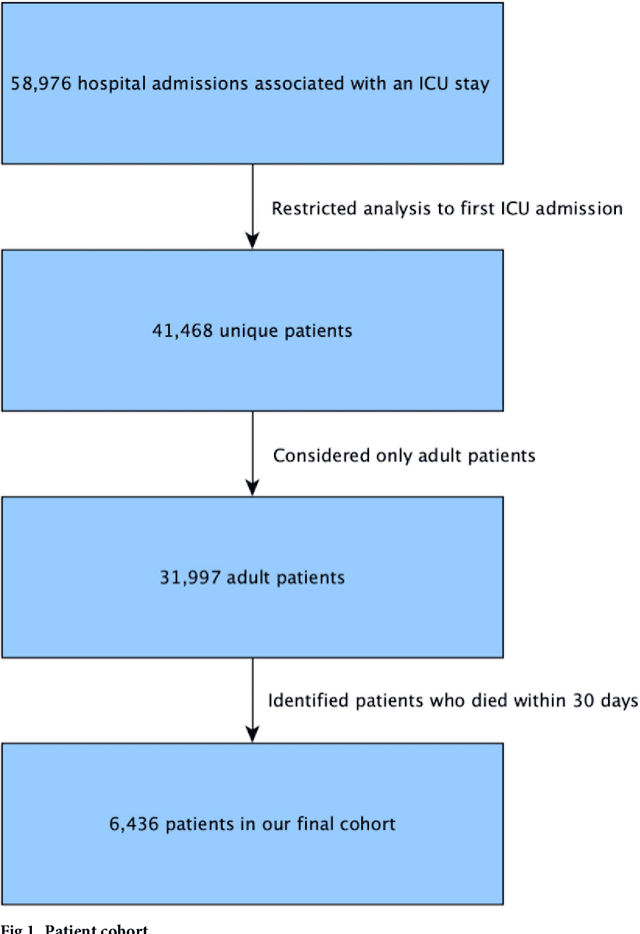
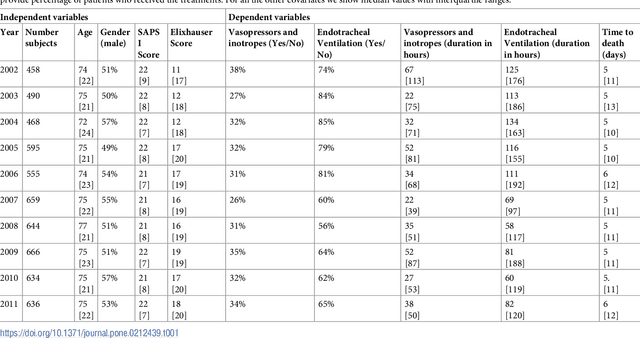
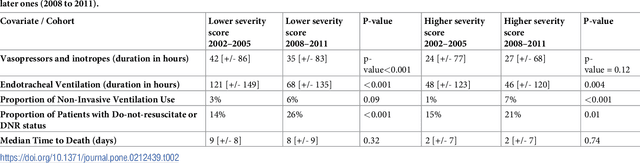
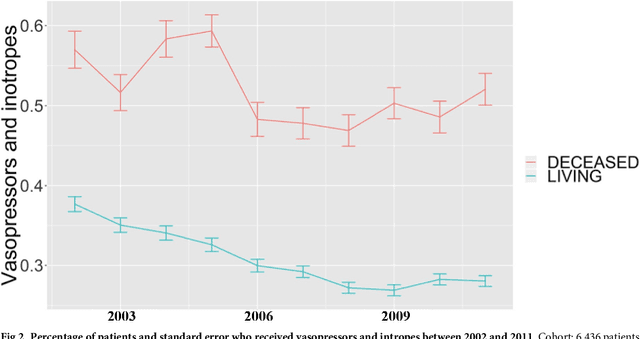
Abstract:Critically ill patients may die despite aggressive treatment. In this study, we examine trends in the application of two such treatments over a decade, as well as the impact of these trends on survival durations in patients who die within a month of ICU admission. We considered observational data available from the MIMIC-III open-access ICU database, collected from June 2001 to October 2012: These data comprise almost 60,000 hospital admissions for a total of 38,645 unique adults. We explored two hypotheses: (i) administration of aggressive treatment during the ICU stay immediately preceding end-of-life would decrease over the study time period and (ii) time-to-death from ICU admission would also decrease due to the decrease in aggressive treatment administration. Tests for significant trends were performed and a p-value threshold of 0.05 was used to assess statistical significance. We found that aggressive treatments in this population were employed with decreasing frequency over the study period duration, and also that reducing aggressive treatments for such patients may not result in shorter times to death. The latter finding has implications for end of life discussions that involve the possible use or non-use of such treatments in those patients with very poor prognosis.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge