Chad Gordon
A Robotic System for Implant Modification in Single-stage Cranioplasty
Jan 12, 2021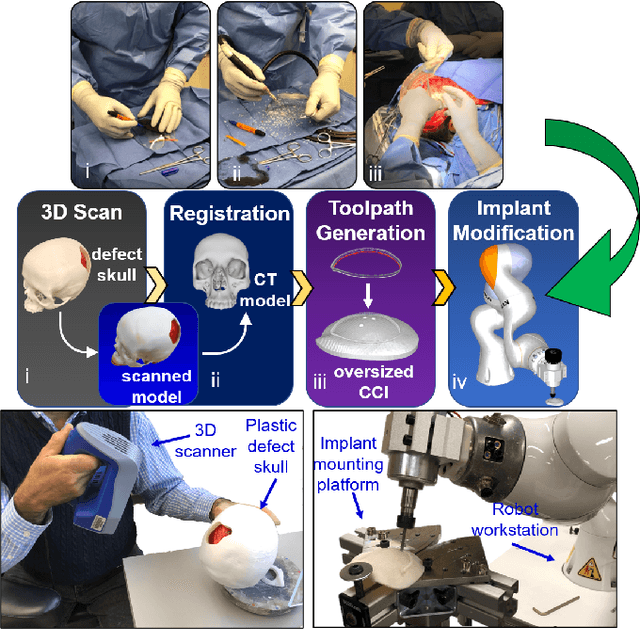
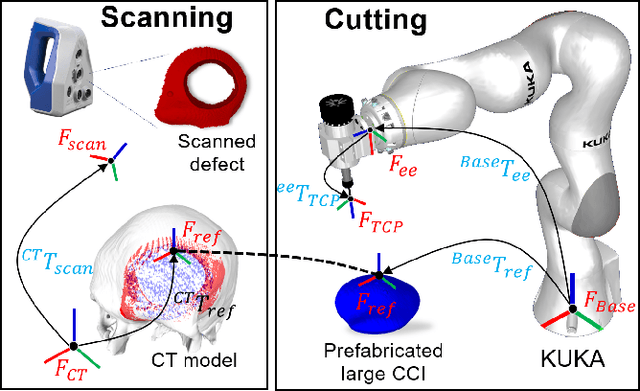
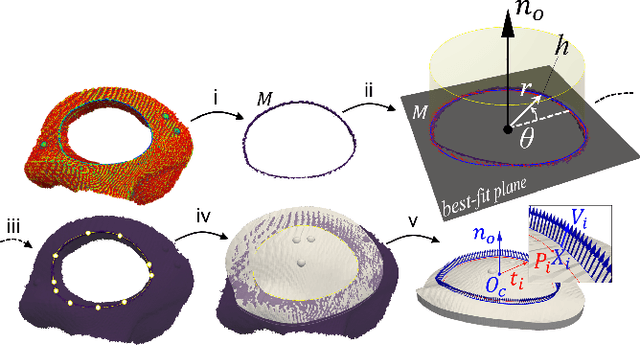
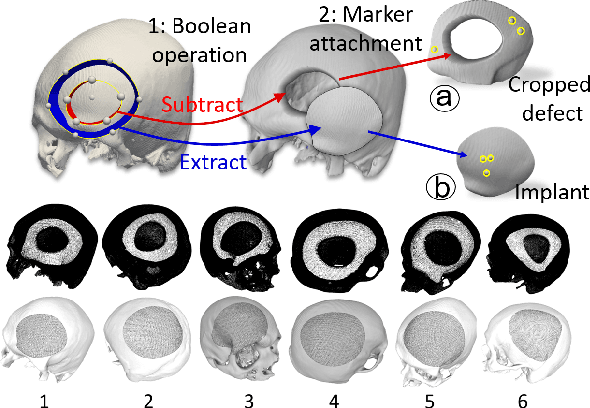
Abstract:Craniomaxillofacial reconstruction with patient-specific customized craniofacial implants (CCIs) is most commonly performed for large-sized skeletal defects. Because the exact size of skull resection may not be known prior to the surgery, in the single-stage cranioplasty, a large CCI is prefabricated and resized intraoperatively with a manual-cutting process provided by a surgeon. The manual resizing, however, may be inaccurate and significantly add to the operating time. This paper introduces a fast and non-contact approach for intraoperatively determining the exact contour of the skull resection and automatically resizing the implant to fit the resection area. Our approach includes four steps: First, a patient's defect information is acquired by a 3D scanner. Second, the scanned defect is aligned to the CCI by registering the scanned defect to the reconstructed CT model. Third, a cutting toolpath is generated from the contour of the scanned defect. Lastly, the large CCI is resized by a cutting robot to fit the resection area according to the given toolpath. To evaluate the resizing performance of our method, six different resection shapes were used in the cutting experiments. We compared the performance of our method to the performances of surgeon's manual resizing and an existing technique which collects the defect contour with an optical tracking system and projects the contour on the CCI to guide the manual modification. The results show that our proposed method improves the resizing accuracy by 56% compared to the surgeon's manual modification and 42% compared to the projection method.
Smooth Extrapolation of Unknown Anatomy via Statistical Shape Models
Sep 23, 2019Abstract:Several methods to perform extrapolation of unknown anatomy were evaluated. The primary application is to enhance surgical procedures that may use partial medical images or medical images of incomplete anatomy. Le Fort-based, face-jaw-teeth transplant is one such procedure. From CT data of 36 skulls and 21 mandibles separate Statistical Shape Models of the anatomical surfaces were created. Using the Statistical Shape Models, incomplete surfaces were projected to obtain complete surface estimates. The surface estimates exhibit non-zero error in regions where the true surface is known; it is desirable to keep the true surface and seamlessly merge the estimated unknown surface. Existing extrapolation techniques produce non-smooth transitions from the true surface to the estimated surface, resulting in additional error and a less aesthetically pleasing result. The three extrapolation techniques evaluated were: copying and pasting of the surface estimate (non-smooth baseline), a feathering between the patient surface and surface estimate, and an estimate generated via a Thin Plate Spline trained from displacements between the surface estimate and corresponding vertices of the known patient surface. Feathering and Thin Plate Spline approaches both yielded smooth transitions. However, feathering corrupted known vertex values. Leave-one-out analyses were conducted, with 5% to 50% of known anatomy removed from the left-out patient and estimated via the proposed approaches. The Thin Plate Spline approach yielded smaller errors than the other two approaches, with an average vertex error improvement of 1.46 mm and 1.38 mm for the skull and mandible respectively, over the baseline approach.
* SPIE Medical Imaging Conference 2015 Paper
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge