Ana M. Barragan-Montero
Dose Prediction with Deep Learning for Prostate Cancer Radiation Therapy: Model Adaptation to Different Treatment Planning Practices
Jun 30, 2020



Abstract:This work aims to study the generalizability of a pre-developed deep learning (DL) dose prediction model for volumetric modulated arc therapy (VMAT) for prostate cancer and to adapt the model to three different internal treatment planning styles and one external institution planning style. We built the source model with planning data from 108 patients previously treated with VMAT for prostate cancer. For the transfer learning, we selected patient cases planned with three different styles from the same institution and one style from a different institution to adapt the source model to four target models. We compared the dose distributions predicted by the source model and the target models with the clinical dose predictions and quantified the improvement in the prediction quality for the target models over the source model using the Dice similarity coefficients (DSC) of 10% to 100% isodose volumes and the dose-volume-histogram (DVH) parameters of the planning target volume and the organs-at-risk. The source model accurately predicts dose distributions for plans generated in the same source style but performs sub-optimally for the three internal and one external target styles, with the mean DSC ranging between 0.81-0.94 and 0.82-0.91 for the internal and the external styles, respectively. With transfer learning, the target model predictions improved the mean DSC to 0.88-0.95 and 0.92-0.96 for the internal and the external styles, respectively. Target model predictions significantly improved the accuracy of the DVH parameter predictions to within 1.6%. We demonstrated model generalizability for DL-based dose prediction and the feasibility of using transfer learning to solve this problem. With 14-29 cases per style, we successfully adapted the source model into several different practice styles. This indicates a realistic way to widespread clinical implementation of DL-based dose prediction.
Three-Dimensional Dose Prediction for Lung IMRT Patients with Deep Neural Networks: Robust Learning from Heterogeneous Beam Configurations
Dec 17, 2018
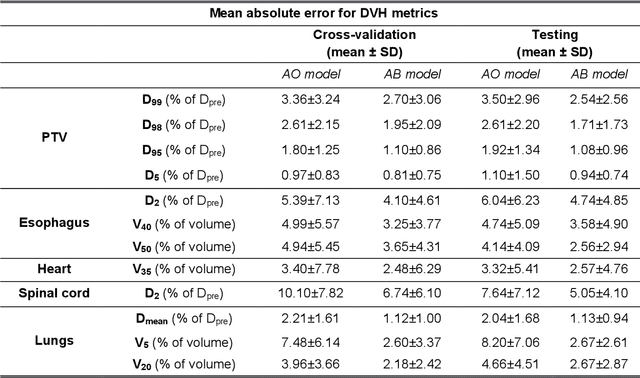
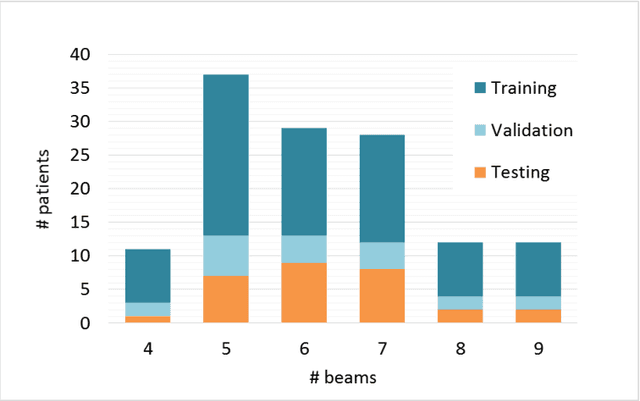
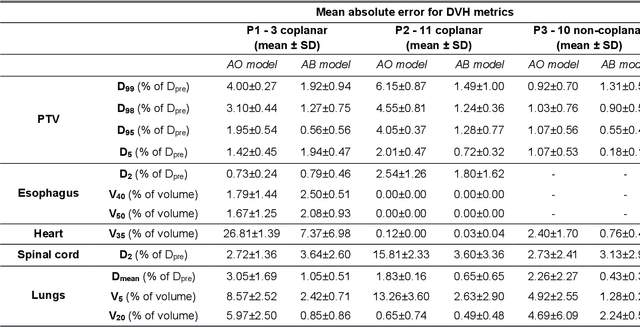
Abstract:The use of neural networks to directly predict three-dimensional dose distributions for automatic planning is becoming popular. However, the existing methods only use patient anatomy as input and assume consistent beam configuration for all patients in the training database. The purpose of this work is to develop a more general model that, in addition to patient anatomy, also considers variable beam configurations, to achieve a more comprehensive automatic planning with a potentially easier clinical implementation, without the need of training specific models for different beam settings.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge