Multi-level Phenotypic Models of Cardiovascular Disease and Obstructive Sleep Apnea Comorbidities: A Longitudinal Wisconsin Sleep Cohort Study
Paper and Code
Jun 19, 2024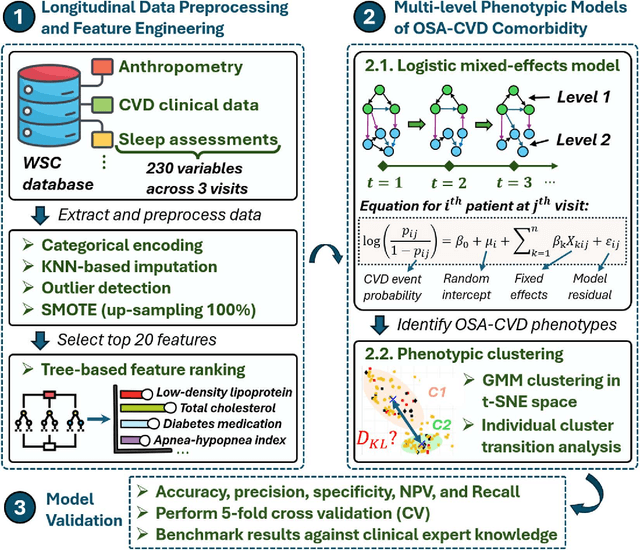
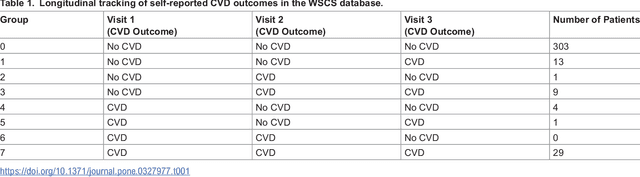
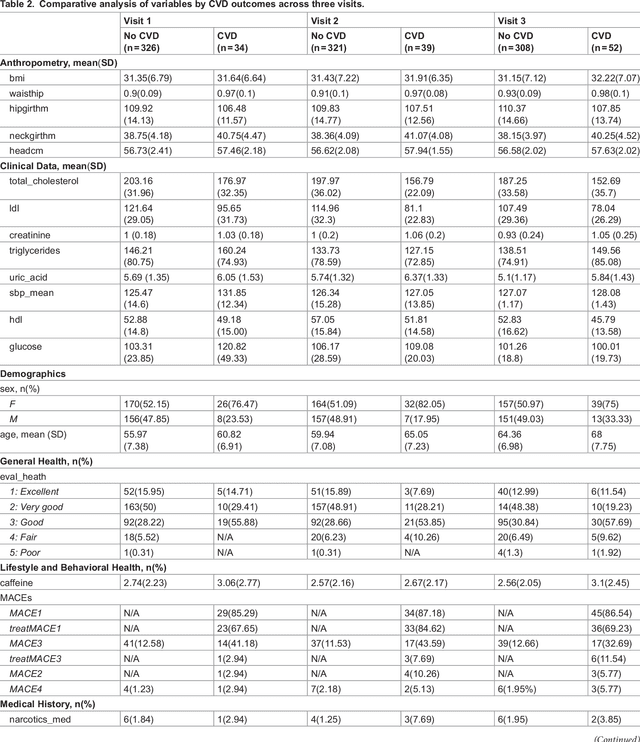
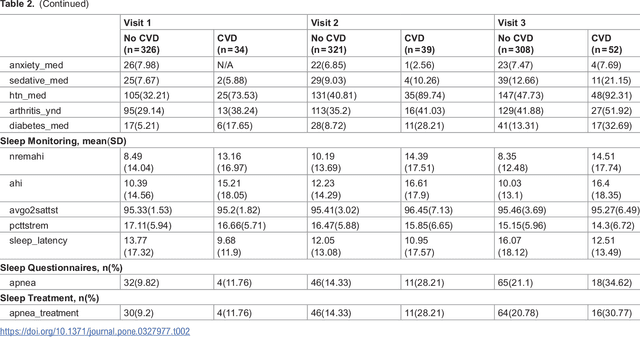
Cardiovascular diseases (CVDs) are notably prevalent among patients with obstructive sleep apnea (OSA), posing unique challenges in predicting CVD progression due to the intricate interactions of comorbidities. Traditional models typically lack the necessary dynamic and longitudinal scope to accurately forecast CVD trajectories in OSA patients. This study introduces a novel multi-level phenotypic model to analyze the progression and interplay of these conditions over time, utilizing data from the Wisconsin Sleep Cohort, which includes 1,123 participants followed for decades. Our methodology comprises three advanced steps: (1) Conducting feature importance analysis through tree-based models to underscore critical predictive variables like total cholesterol, low-density lipoprotein (LDL), and diabetes. (2) Developing a logistic mixed-effects model (LGMM) to track longitudinal transitions and pinpoint significant factors, which displayed a diagnostic accuracy of 0.9556. (3) Implementing t-distributed Stochastic Neighbor Embedding (t-SNE) alongside Gaussian Mixture Models (GMM) to segment patient data into distinct phenotypic clusters that reflect varied risk profiles and disease progression pathways. This phenotypic clustering revealed two main groups, with one showing a markedly increased risk of major adverse cardiovascular events (MACEs), underscored by the significant predictive role of nocturnal hypoxia and sympathetic nervous system activity from sleep data. Analysis of transitions and trajectories with t-SNE and GMM highlighted different progression rates within the cohort, with one cluster progressing more slowly towards severe CVD states than the other. This study offers a comprehensive understanding of the dynamic relationship between CVD and OSA, providing valuable tools for predicting disease onset and tailoring treatment approaches.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge