Tiago Oliveira
Connecting metrics for shape-texture knowledge in computer vision
Jan 25, 2023Abstract:Modern artificial neural networks, including convolutional neural networks and vision transformers, have mastered several computer vision tasks, including object recognition. However, there are many significant differences between the behavior and robustness of these systems and of the human visual system. Deep neural networks remain brittle and susceptible to many changes in the image that do not cause humans to misclassify images. Part of this different behavior may be explained by the type of features humans and deep neural networks use in vision tasks. Humans tend to classify objects according to their shape while deep neural networks seem to rely mostly on texture. Exploring this question is relevant, since it may lead to better performing neural network architectures and to a better understanding of the workings of the vision system of primates. In this work, we advance the state of the art in our understanding of this phenomenon, by extending previous analyses to a much larger set of deep neural network architectures. We found that the performance of models in image classification tasks is highly correlated with their shape bias measured at the output and penultimate layer. Furthermore, our results showed that the number of neurons that represent shape and texture are strongly anti-correlated, thus providing evidence that there is competition between these two types of features. Finally, we observed that while in general there is a correlation between performance and shape bias, there are significant variations between architecture families.
Resolving Conflicts in Clinical Guidelines using Argumentation
Feb 20, 2019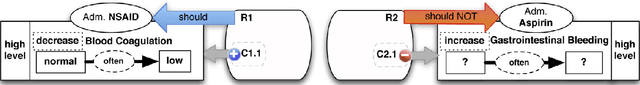
Abstract:Automatically reasoning with conflicting generic clinical guidelines is a burning issue in patient-centric medical reasoning where patient-specific conditions and goals need to be taken into account. It is even more challenging in the presence of preferences such as patient's wishes and clinician's priorities over goals. We advance a structured argumentation formalism for reasoning with conflicting clinical guidelines, patient-specific information and preferences. Our formalism integrates assumption-based reasoning and goal-driven selection among reasoning outcomes. Specifically, we assume applicability of guideline recommendations concerning the generic goal of patient well-being, resolve conflicts among recommendations using patient's conditions and preferences, and then consider prioritised patient-centered goals to yield non-conflicting, goal-maximising and preference-respecting recommendations. We rely on the state-of-the-art Transition-based Medical Recommendation model for representing guideline recommendations and augment it with context given by the patient's conditions, goals, as well as preferences over recommendations and goals. We establish desirable properties of our approach in terms of sensitivity to recommendation conflicts and patient context.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge