Ricardo Coimbra Brioso
ARTInp: CBCT-to-CT Image Inpainting and Image Translation in Radiotherapy
Feb 07, 2025



Abstract:A key step in Adaptive Radiation Therapy (ART) workflows is the evaluation of the patient's anatomy at treatment time to ensure the accuracy of the delivery. To this end, Cone Beam Computerized Tomography (CBCT) is widely used being cost-effective and easy to integrate into the treatment process. Nonetheless, CBCT images have lower resolution and more artifacts than CT scans, making them less reliable for precise treatment validation. Moreover, in complex treatments such as Total Marrow and Lymph Node Irradiation (TMLI), where full-body visualization of the patient is critical for accurate dose delivery, the CBCT images are often discontinuous, leaving gaps that could contain relevant anatomical information. To address these limitations, we propose ARTInp (Adaptive Radiation Therapy Inpainting), a novel deep-learning framework combining image inpainting and CBCT-to-CT translation. ARTInp employs a dual-network approach: a completion network that fills anatomical gaps in CBCT volumes and a custom Generative Adversarial Network (GAN) to generate high-quality synthetic CT (sCT) images. We trained ARTInp on a dataset of paired CBCT and CT images from the SynthRad 2023 challenge, and the performance achieved on a test set of 18 patients demonstrates its potential for enhancing CBCT-based workflows in radiotherapy.
Investigating Gender Bias in Lymph-node Segmentation with Anatomical Priors
Sep 24, 2024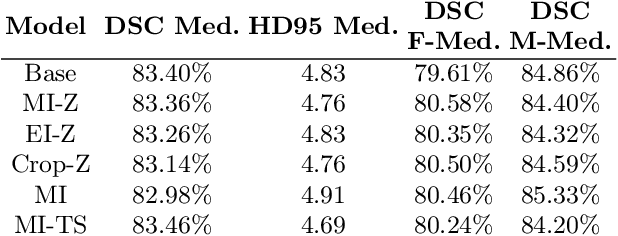
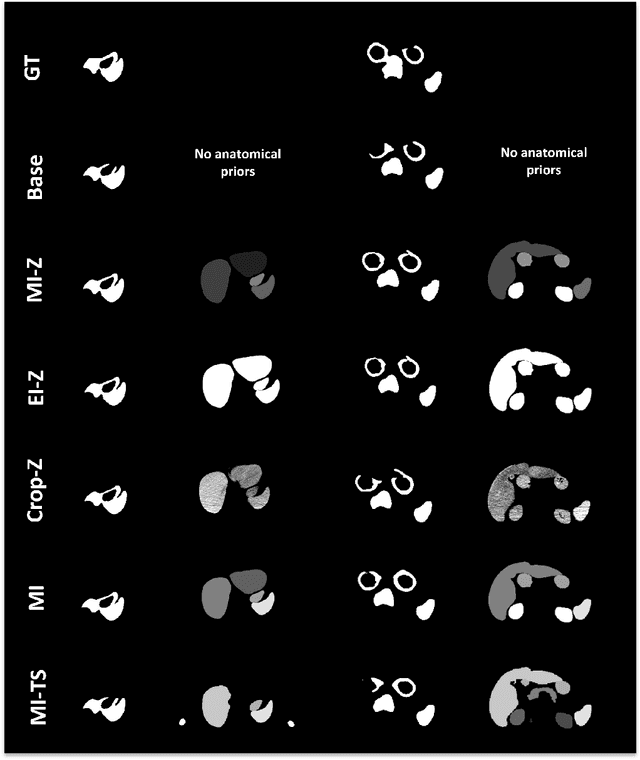
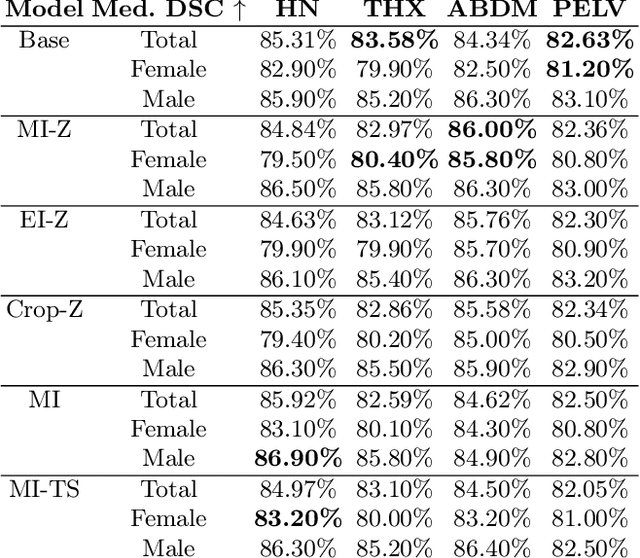
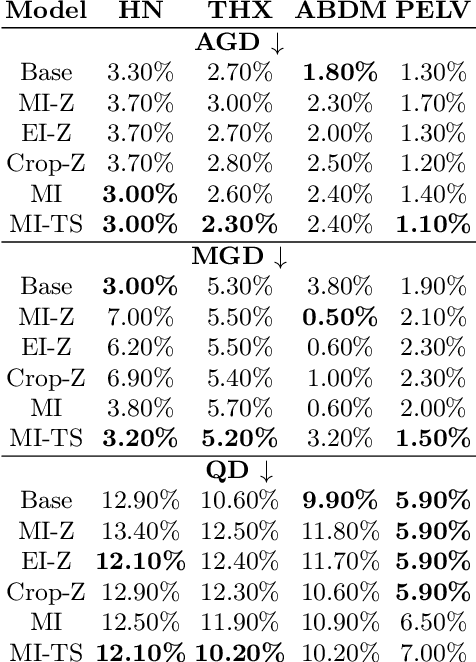
Abstract:Radiotherapy requires precise segmentation of organs at risk (OARs) and of the Clinical Target Volume (CTV) to maximize treatment efficacy and minimize toxicity. While deep learning (DL) has significantly advanced automatic contouring, complex targets like CTVs remain challenging. This study explores the use of simpler, well-segmented structures (e.g., OARs) as Anatomical Prior (AP) information to improve CTV segmentation. We investigate gender bias in segmentation models and the mitigation effect of the prior information. Findings indicate that incorporating prior knowledge with the discussed strategies enhances segmentation quality in female patients and reduces gender bias, particularly in the abdomen region. This research provides a comparative analysis of new encoding strategies and highlights the potential of using AP to achieve fairer segmentation outcomes.
Deep Learning-Based Auto-Segmentation of Planning Target Volume for Total Marrow and Lymph Node Irradiation
Feb 09, 2024



Abstract:In order to optimize the radiotherapy delivery for cancer treatment, especially when dealing with complex treatments such as Total Marrow and Lymph Node Irradiation (TMLI), the accurate contouring of the Planning Target Volume (PTV) is crucial. Unfortunately, relying on manual contouring for such treatments is time-consuming and prone to errors. In this paper, we investigate the application of Deep Learning (DL) to automate the segmentation of the PTV in TMLI treatment, building upon previous work that introduced a solution to this problem based on a 2D U-Net model. We extend the previous research (i) by employing the nnU-Net framework to develop both 2D and 3D U-Net models and (ii) by evaluating the trained models on the PTV with the exclusion of bones, which consist mainly of lymp-nodes and represent the most challenging region of the target volume to segment. Our result show that the introduction of nnU-NET framework led to statistically significant improvement in the segmentation performance. In addition, the analysis on the PTV after the exclusion of bones showed that the models are quite robust also on the most challenging areas of the target volume. Overall, our study is a significant step forward in the application of DL in a complex radiotherapy treatment such as TMLI, offering a viable and scalable solution to increase the number of patients who can benefit from this treatment.
Segmentation of Planning Target Volume in CT Series for Total Marrow Irradiation Using U-Net
Apr 05, 2023



Abstract:Radiotherapy (RT) is a key component in the treatment of various cancers, including Acute Lymphocytic Leukemia (ALL) and Acute Myelogenous Leukemia (AML). Precise delineation of organs at risk (OARs) and target areas is essential for effective treatment planning. Intensity Modulated Radiotherapy (IMRT) techniques, such as Total Marrow Irradiation (TMI) and Total Marrow and Lymph node Irradiation (TMLI), provide more precise radiation delivery compared to Total Body Irradiation (TBI). However, these techniques require time-consuming manual segmentation of structures in Computerized Tomography (CT) scans by the Radiation Oncologist (RO). In this paper, we present a deep learning-based auto-contouring method for segmenting Planning Target Volume (PTV) for TMLI treatment using the U-Net architecture. We trained and compared two segmentation models with two different loss functions on a dataset of 100 patients treated with TMLI at the Humanitas Research Hospital between 2011 and 2021. Despite challenges in lymph node areas, the best model achieved an average Dice score of 0.816 for PTV segmentation. Our findings are a preliminary but significant step towards developing a segmentation model that has the potential to save radiation oncologists a considerable amount of time. This could allow for the treatment of more patients, resulting in improved clinical practice efficiency and more reproducible contours.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge