Qingqing Mao
OpenMedLM: Prompt engineering can out-perform fine-tuning in medical question-answering with open-source large language models
Feb 29, 2024Abstract:LLMs have become increasingly capable at accomplishing a range of specialized-tasks and can be utilized to expand equitable access to medical knowledge. Most medical LLMs have involved extensive fine-tuning, leveraging specialized medical data and significant, thus costly, amounts of computational power. Many of the top performing LLMs are proprietary and their access is limited to very few research groups. However, open-source (OS) models represent a key area of growth for medical LLMs due to significant improvements in performance and an inherent ability to provide the transparency and compliance required in healthcare. We present OpenMedLM, a prompting platform which delivers state-of-the-art (SOTA) performance for OS LLMs on medical benchmarks. We evaluated a range of OS foundation LLMs (7B-70B) on four medical benchmarks (MedQA, MedMCQA, PubMedQA, MMLU medical-subset). We employed a series of prompting strategies, including zero-shot, few-shot, chain-of-thought (random selection and kNN selection), and ensemble/self-consistency voting. We found that OpenMedLM delivers OS SOTA results on three common medical LLM benchmarks, surpassing the previous best performing OS models that leveraged computationally costly extensive fine-tuning. The model delivers a 72.6% accuracy on the MedQA benchmark, outperforming the previous SOTA by 2.4%, and achieves 81.7% accuracy on the MMLU medical-subset, establishing itself as the first OS LLM to surpass 80% accuracy on this benchmark. Our results highlight medical-specific emergent properties in OS LLMs which have not yet been documented to date elsewhere, and showcase the benefits of further leveraging prompt engineering to improve the performance of accessible LLMs for medical applications.
Optimal discharge of patients from intensive care via a data-driven policy learning framework
Dec 17, 2021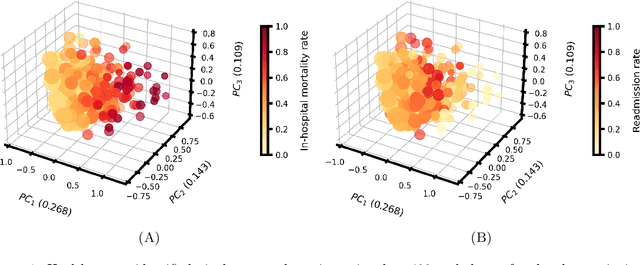
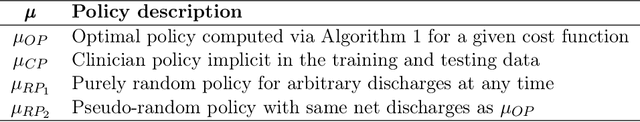

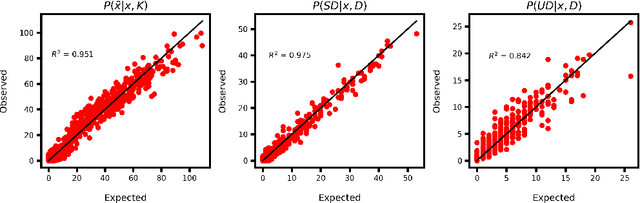
Abstract:Clinical decision support tools rooted in machine learning and optimization can provide significant value to healthcare providers, including through better management of intensive care units. In particular, it is important that the patient discharge task addresses the nuanced trade-off between decreasing a patient's length of stay (and associated hospitalization costs) and the risk of readmission or even death following the discharge decision. This work introduces an end-to-end general framework for capturing this trade-off to recommend optimal discharge timing decisions given a patient's electronic health records. A data-driven approach is used to derive a parsimonious, discrete state space representation that captures a patient's physiological condition. Based on this model and a given cost function, an infinite-horizon discounted Markov decision process is formulated and solved numerically to compute an optimal discharge policy, whose value is assessed using off-policy evaluation strategies. Extensive numerical experiments are performed to validate the proposed framework using real-life intensive care unit patient data.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge