Per Munck af Rosenschöld
Radiation Physics, Department of Hematology, Oncology and Radiation Physics, Skåne University Hospital, Lund, Sweden
LUND-PROBE -- LUND Prostate Radiotherapy Open Benchmarking and Evaluation dataset
Feb 06, 2025Abstract:Radiotherapy treatment for prostate cancer relies on computed tomography (CT) and/or magnetic resonance imaging (MRI) for segmentation of target volumes and organs at risk (OARs). Manual segmentation of these volumes is regarded as the gold standard for ground truth in machine learning applications but to acquire such data is tedious and time-consuming. A publicly available clinical dataset is presented, comprising MRI- and synthetic CT (sCT) images, target and OARs segmentations, and radiotherapy dose distributions for 432 prostate cancer patients treated with MRI-guided radiotherapy. An extended dataset with 35 patients is also included, with the addition of deep learning (DL)-generated segmentations, DL segmentation uncertainty maps, and DL segmentations manually adjusted by four radiation oncologists. The publication of these resources aims to aid research within the fields of automated radiotherapy treatment planning, segmentation, inter-observer analyses, and DL model uncertainty investigation. The dataset is hosted on the AIDA Data Hub and offers a free-to-use resource for the scientific community, valuable for the advancement of medical imaging and prostate cancer radiotherapy research.
A Modality-Adaptive Method for Segmenting Brain Tumors and Organs-at-Risk in Radiation Therapy Planning
Aug 15, 2018
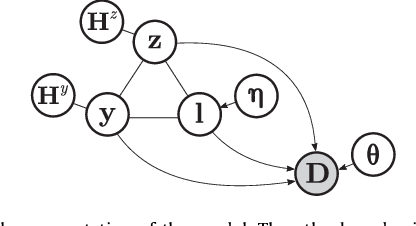
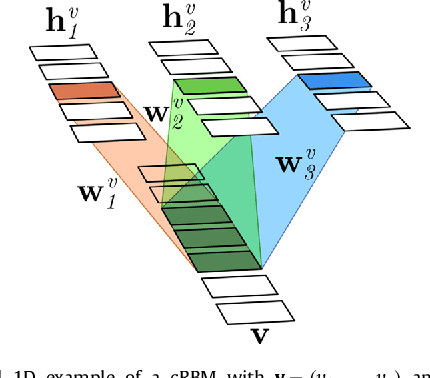

Abstract:In this paper we present a method for simultaneously segmenting brain tumors and an extensive set of organs-at-risk for radiation therapy planning of glioblastomas. The method combines a contrast-adaptive generative model for whole-brain segmentation with a new spatial regularization model of tumor shape using convolutional restricted Boltzmann machines. We demonstrate experimentally that the method is able to adapt to image acquisitions that differ substantially from any available training data, ensuring its applicability across treatment sites; that its tumor segmentation accuracy is comparable to that of the current state of the art; and that it captures most organs-at-risk sufficiently well for radiation therapy planning purposes. The proposed method may be a valuable step towards automating the delineation of brain tumors and organs-at-risk in glioblastoma patients undergoing radiation therapy.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge