Mark Alberti
Corneal Pachymetry by AS-OCT after Descemet's Membrane Endothelial Keratoplasty
Feb 15, 2021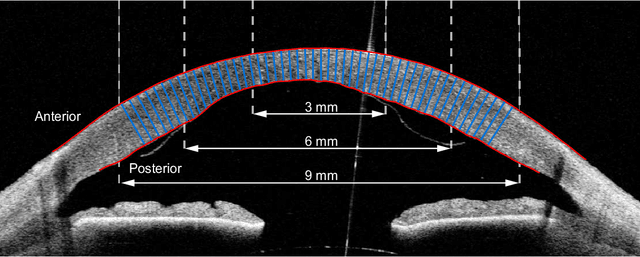
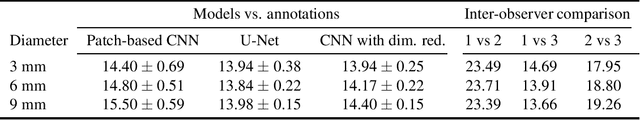
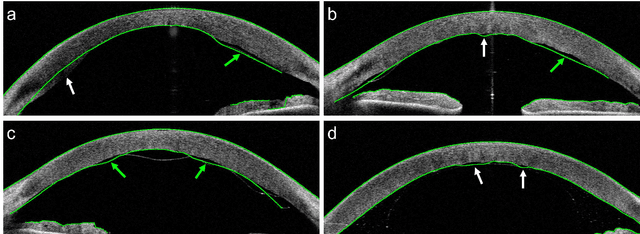
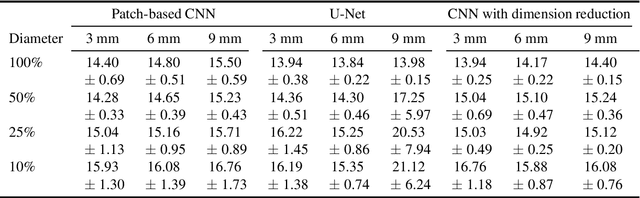
Abstract:Corneal thickness (pachymetry) maps can be used to monitor restoration of corneal endothelial function, for example after Descemet's membrane endothelial keratoplasty (DMEK). Automated delineation of the corneal interfaces in anterior segment optical coherence tomography (AS-OCT) can be challenging for corneas that are irregularly shaped due to pathology, or as a consequence of surgery, leading to incorrect thickness measurements. In this research, deep learning is used to automatically delineate the corneal interfaces and measure corneal thickness with high accuracy in post-DMEK AS-OCT B-scans. Three different deep learning strategies were developed based on 960 B-scans from 68 patients. On an independent test set of 320 B-scans, corneal thickness could be measured with an error of 13.98 to 15.50 micrometer for the central 9 mm range, which is less than 3% of the average corneal thickness. The accurate thickness measurements were used to construct detailed pachymetry maps. Moreover, follow-up scans could be registered based on anatomical landmarks to obtain differential pachymetry maps. These maps may enable a more comprehensive understanding of the restoration of the endothelial function after DMEK, where thickness often varies throughout different regions of the cornea, and subsequently contribute to a standardized postoperative regime.
Quantifying Graft Detachment after Descemet's Membrane Endothelial Keratoplasty with Deep Convolutional Neural Networks
Apr 24, 2020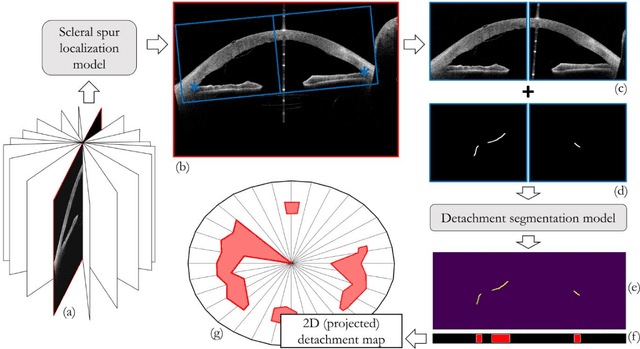
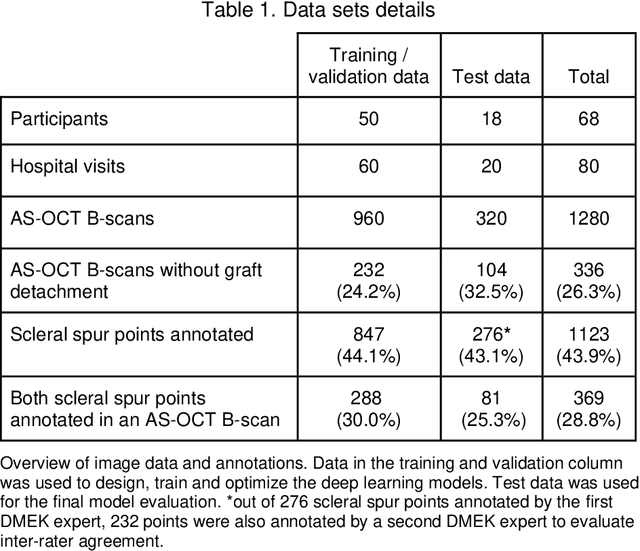
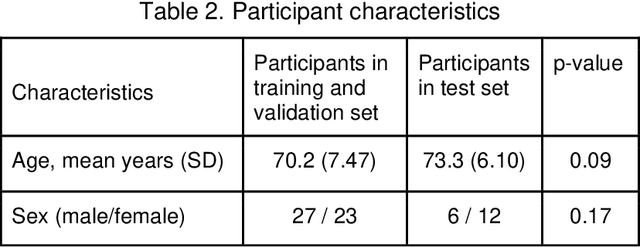
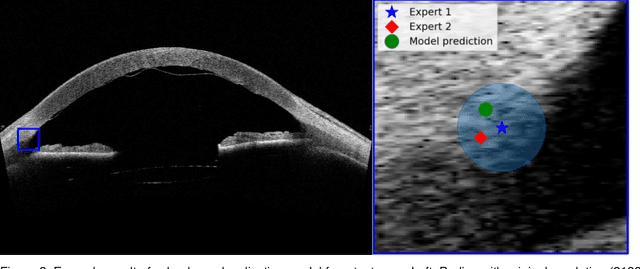
Abstract:Purpose: We developed a method to automatically locate and quantify graft detachment after Descemet's Membrane Endothelial Keratoplasty (DMEK) in Anterior Segment Optical Coherence Tomography (AS-OCT) scans. Methods: 1280 AS-OCT B-scans were annotated by a DMEK expert. Using the annotations, a deep learning pipeline was developed to localize scleral spur, center the AS-OCT B-scans and segment the detached graft sections. Detachment segmentation model performance was evaluated per B-scan by comparing (1) length of detachment and (2) horizontal projection of the detached sections with the expert annotations. Horizontal projections were used to construct graft detachment maps. All final evaluations were done on a test set that was set apart during training of the models. A second DMEK expert annotated the test set to determine inter-rater performance. Results: Mean scleral spur localization error was 0.155 mm, whereas the inter-rater difference was 0.090 mm. The estimated graft detachment lengths were in 69% of the cases within a 10-pixel (~150{\mu}m) difference from the ground truth (77% for the second DMEK expert). Dice scores for the horizontal projections of all B-scans with detachments were 0.896 and 0.880 for our model and the second DMEK expert respectively. Conclusion: Our deep learning model can be used to automatically and instantly localize graft detachment in AS-OCT B-scans. Horizontal detachment projections can be determined with the same accuracy as a human DMEK expert, allowing for the construction of accurate graft detachment maps. Translational Relevance: Automated localization and quantification of graft detachment can support DMEK research and standardize clinical decision making.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge