Mélina Khansari
Density-based Isometric Mapping
Mar 04, 2024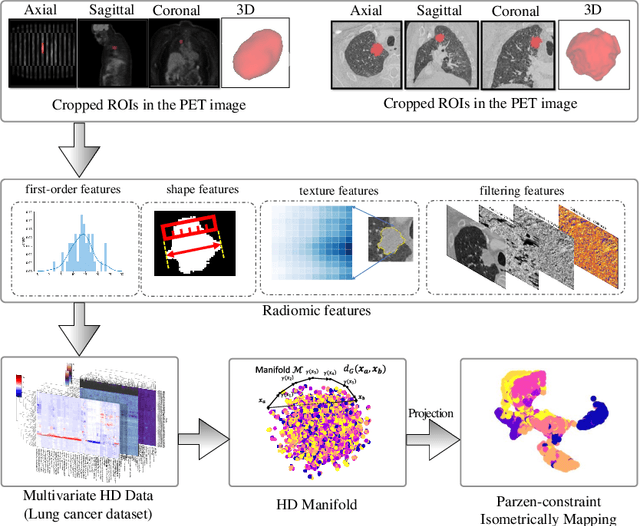
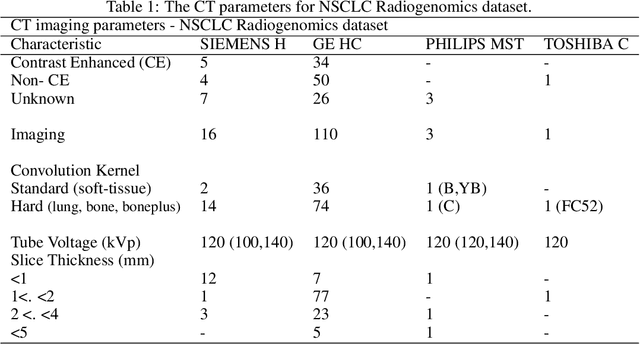
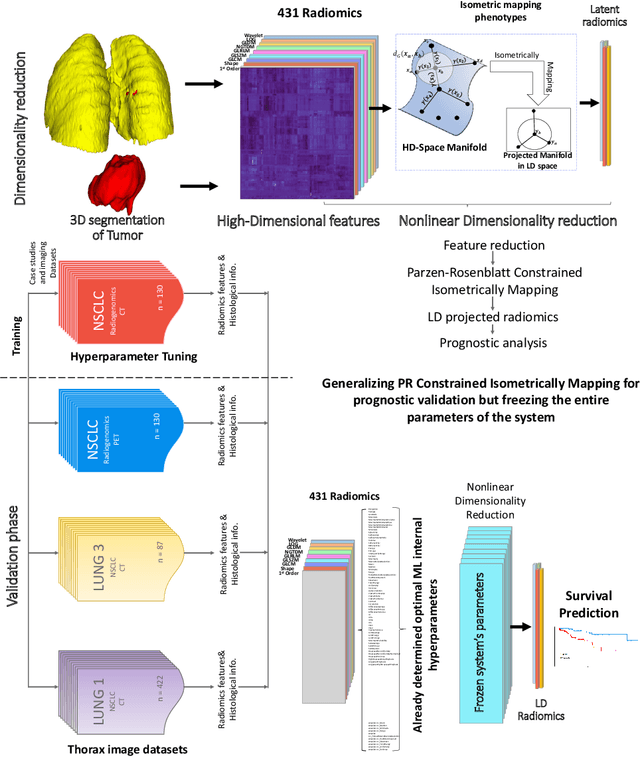
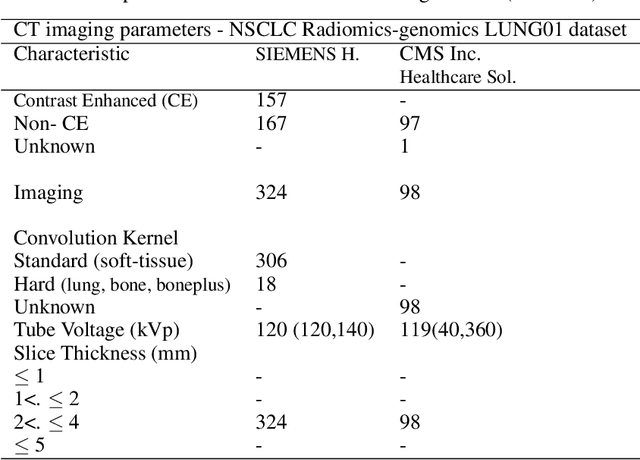
Abstract:The isometric mapping method employs the shortest path algorithm to estimate the Euclidean distance between points on High dimensional (HD) manifolds. This may not be sufficient for weakly uniformed HD data as it could lead to overestimating distances between far neighboring points, resulting in inconsistencies between the intrinsic (local) and extrinsic (global) distances during the projection. To address this issue, we modify the shortest path algorithm by adding a novel constraint inspired by the Parzen-Rosenblatt (PR) window, which helps to maintain the uniformity of the constructed shortest-path graph in Isomap. Multiple imaging datasets overall of 72,236 cases, 70,000 MINST data, 1596 from multiple Chest-XRay pneumonia datasets, and three NSCLC CT/PET datasets with a total of 640 lung cancer patients, were used to benchmark and validate PR-Isomap. 431 imaging biomarkers were extracted from each modality. Our results indicate that PR-Isomap projects HD attributes into a lower-dimensional (LD) space while preserving information, visualized by the MNIST dataset indicating the maintaining local and global distances. PR-Isomap achieved the highest comparative accuracies of 80.9% (STD:5.8) for pneumonia and 78.5% (STD:4.4), 88.4% (STD:1.4), and 61.4% (STD:11.4) for three NSCLC datasets, with a confidence interval of 95% for outcome prediction. Similarly, the multivariate Cox model showed higher overall survival, measured with c-statistics and log-likelihood test, of PR-Isomap compared to other dimensionality reduction methods. Kaplan Meier survival curve also signifies the notable ability of PR-Isomap to distinguish between high-risk and low-risk patients using multimodal imaging biomarkers preserving HD imaging characteristics for precision medicine.
AI-Enabled Lung Cancer Prognosis
Feb 12, 2024Abstract:Lung cancer is the primary cause of cancer-related mortality, claiming approximately 1.79 million lives globally in 2020, with an estimated 2.21 million new cases diagnosed within the same period. Among these, Non-Small Cell Lung Cancer (NSCLC) is the predominant subtype, characterized by a notably bleak prognosis and low overall survival rate of approximately 25% over five years across all disease stages. However, survival outcomes vary considerably based on the stage at diagnosis and the therapeutic interventions administered. Recent advancements in artificial intelligence (AI) have revolutionized the landscape of lung cancer prognosis. AI-driven methodologies, including machine learning and deep learning algorithms, have shown promise in enhancing survival prediction accuracy by efficiently analyzing complex multi-omics data and integrating diverse clinical variables. By leveraging AI techniques, clinicians can harness comprehensive prognostic insights to tailor personalized treatment strategies, ultimately improving patient outcomes in NSCLC. Overviewing AI-driven data processing can significantly help bolster the understanding and provide better directions for using such systems.
* This is the author's version of a book chapter entitled: "Cancer Research: An Interdisciplinary Approach", Springer
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge