John A. Shepherd
Deep Learning Enables Large-Scale Shape and Appearance Modeling in Total-Body DXA Imaging
Aug 13, 2025Abstract:Total-body dual X-ray absorptiometry (TBDXA) imaging is a relatively low-cost whole-body imaging modality, widely used for body composition assessment. We develop and validate a deep learning method for automatic fiducial point placement on TBDXA scans using 1,683 manually-annotated TBDXA scans. The method achieves 99.5% percentage correct keypoints in an external testing dataset. To demonstrate the value for shape and appearance modeling (SAM), our method is used to place keypoints on 35,928 scans for five different TBDXA imaging modes, then associations with health markers are tested in two cohorts not used for SAM model generation using two-sample Kolmogorov-Smirnov tests. SAM feature distributions associated with health biomarkers are shown to corroborate existing evidence and generate new hypotheses on body composition and shape's relationship to various frailty, metabolic, inflammation, and cardiometabolic health markers. Evaluation scripts, model weights, automatic point file generation code, and triangulation files are available at https://github.com/hawaii-ai/dxa-pointplacement.
Artificial Intelligence-Informed Handheld Breast Ultrasound for Screening: A Systematic Review of Diagnostic Test Accuracy
Nov 11, 2024



Abstract:Background. Breast cancer screening programs using mammography have led to significant mortality reduction in high-income countries. However, many low- and middle-income countries lack resources for mammographic screening. Handheld breast ultrasound (BUS) is a low-cost alternative but requires substantial training. Artificial intelligence (AI) enabled BUS may aid in both the detection (perception) and classification (interpretation) of breast cancer. Materials and Methods. This review (CRD42023493053) is reported in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) and SWiM (Synthesis Without Meta-analysis) guidelines. PubMed and Google Scholar were searched from January 1, 2016 to December 12, 2023. A meta-analysis was not attempted. Studies are grouped according to their AI task type, application time, and AI task. Study quality is assessed using the QUality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) tool. Results. Of 763 candidate studies, 314 total full texts were reviewed. 34 studies are included. The AI tasks of included studies are as follows: 1 frame selection, 6 detection, 11 segmentation, and 16 classification. In total, 5.7 million BUS images from over 185,000 patients were used for AI training or validation. A single study included a prospective testing set. 79% of studies were at high or unclear risk of bias. Conclusion. There has been encouraging development of AI for BUS. Despite studies demonstrating high performance across all identified tasks, the evidence supporting AI-enhanced BUS generally lacks robustness. High-quality model validation will be key to realizing the potential for AI-enhanced BUS in increasing access to screening in resource-limited environments.
Deep Learning Predicts Mammographic Breast Density in Clinical Breast Ultrasound Images
Oct 31, 2024



Abstract:Background: Mammographic breast density, as defined by the American College of Radiology's Breast Imaging Reporting and Data System (BI-RADS), is one of the strongest risk factors for breast cancer, but is derived from mammographic images. Breast ultrasound (BUS) is an alternative breast cancer screening modality, particularly useful for early detection in low-resource, rural contexts. The purpose of this study was to explore an artificial intelligence (AI) model to predict BI-RADS mammographic breast density category from clinical, handheld BUS imaging. Methods: All data are sourced from the Hawaii and Pacific Islands Mammography Registry. We compared deep learning methods from BUS imaging, as well as machine learning models from image statistics alone. The use of AI-derived BUS density as a risk factor for breast cancer was then compared to clinical BI-RADS breast density while adjusting for age. The BUS data were split by individual into 70/20/10% groups for training, validation, and testing. Results: 405,120 clinical BUS images from 14.066 women were selected for inclusion in this study, resulting in 9.846 women for training (302,574 images), 2,813 for validation (11,223 images), and 1,406 for testing (4,042 images). On the held-out testing set, the strongest AI model achieves AUROC 0.854 predicting BI-RADS mammographic breast density from BUS imaging and outperforms all shallow machine learning methods based on image statistics. In cancer risk prediction, age-adjusted AI BUS breast density predicted 5-year breast cancer risk with 0.633 AUROC, as compared to 0.637 AUROC from age-adjusted clinical breast density. Conclusions: BI-RADS mammographic breast density can be estimated from BUS imaging with high accuracy using a deep learning model. Furthermore, we demonstrate that AI-derived BUS breast density is predictive of 5-year breast cancer risk in our population.
BUSClean: Open-source software for breast ultrasound image pre-processing and knowledge extraction for medical AI
Jul 16, 2024Abstract:Development of artificial intelligence (AI) for medical imaging demands curation and cleaning of large-scale clinical datasets comprising hundreds of thousands of images. Some modalities, such as mammography, contain highly standardized imaging. In contrast, breast ultrasound imaging (BUS) can contain many irregularities not indicated by scan metadata, such as enhanced scan modes, sonographer annotations, or additional views. We present an open-source software solution for automatically processing clinical BUS datasets. The algorithm performs BUS scan filtering, cleaning, and knowledge extraction from sonographer annotations. Its modular design enables users to adapt it to new settings. Experiments on an internal testing dataset of 430 clinical BUS images achieve >95% sensitivity and >98% specificity in detecting every type of text annotation, >98% sensitivity and specificity in detecting scans with blood flow highlighting, alternative scan modes, or invalid scans. A case study on a completely external, public dataset of BUS scans found that BUSClean identified text annotations and scans with blood flow highlighting with 88.6% and 90.9% sensitivity and 98.3% and 99.9% specificity, respectively. Adaptation of the lesion caliper detection method to account for a type of caliper specific to the case study demonstrates intended use of BUSClean in new data distributions and improved performance in lesion caliper detection from 43.3% and 93.3% out-of-the-box to 92.1% and 92.3% sensitivity and specificity, respectively. Source code, example notebooks, and sample data are available at https://github.com/hawaii-ai/bus-cleaning.
Learning a Clinically-Relevant Concept Bottleneck for Lesion Detection in Breast Ultrasound
Jun 29, 2024Abstract:Detecting and classifying lesions in breast ultrasound images is a promising application of artificial intelligence (AI) for reducing the burden of cancer in regions with limited access to mammography. Such AI systems are more likely to be useful in a clinical setting if their predictions can be explained to a radiologist. This work proposes an explainable AI model that provides interpretable predictions using a standard lexicon from the American College of Radiology's Breast Imaging and Reporting Data System (BI-RADS). The model is a deep neural network featuring a concept bottleneck layer in which known BI-RADS features are predicted before making a final cancer classification. This enables radiologists to easily review the predictions of the AI system and potentially fix errors in real time by modifying the concept predictions. In experiments, a model is developed on 8,854 images from 994 women with expert annotations and histological cancer labels. The model outperforms state-of-the-art lesion detection frameworks with 48.9 average precision on the held-out testing set, and for cancer classification, concept intervention is shown to increase performance from 0.876 to 0.885 area under the receiver operating characteristic curve. Training and evaluation code is available at https://github.com/hawaii-ai/bus-cbm.
Quantitative Imaging Principles Improves Medical Image Learning
Jun 14, 2022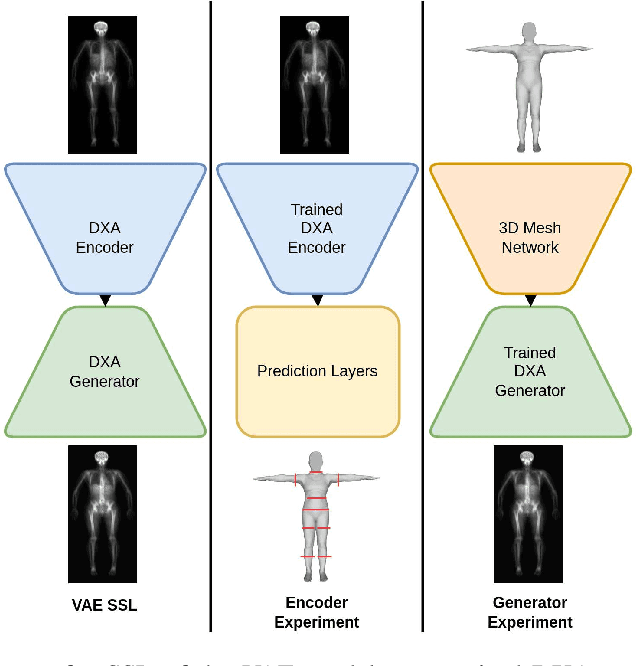
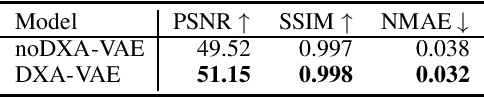
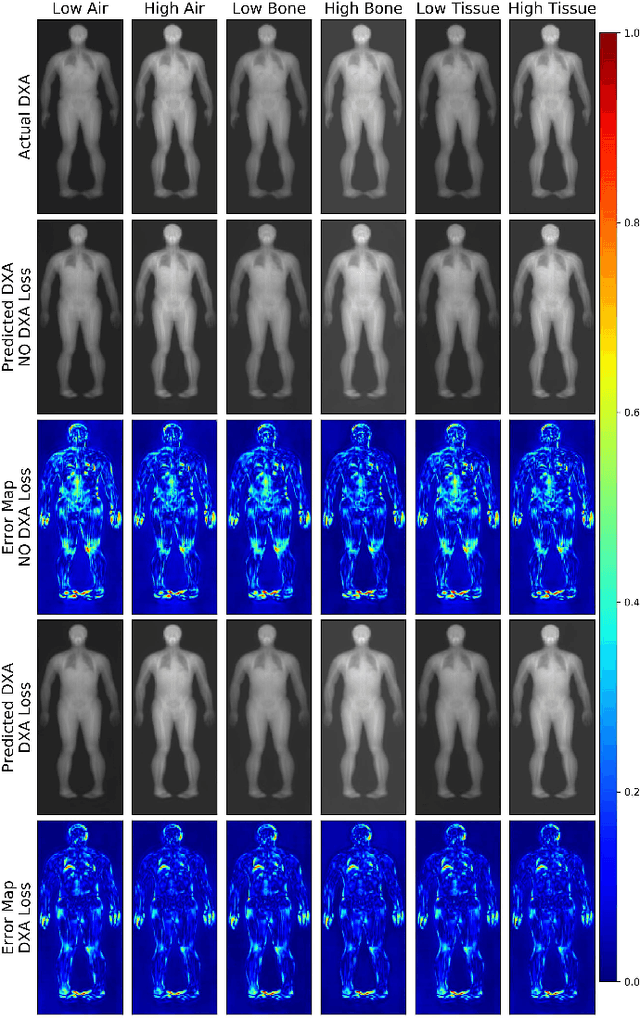
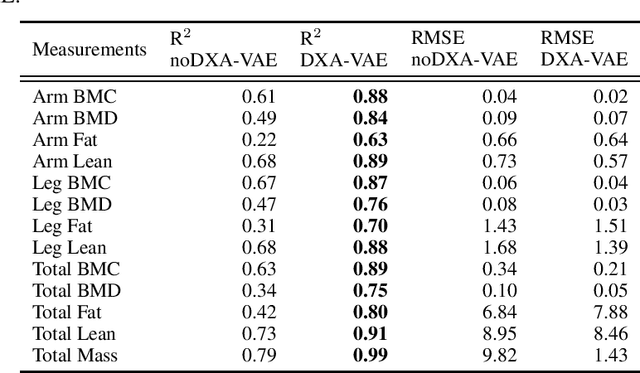
Abstract:Fundamental differences between natural and medical images have recently favored the use of self-supervised learning (SSL) over ImageNet transfer learning for medical image applications. Differences between image types are primarily due to the imaging modality and medical images utilize a wide range of physics based techniques while natural images are captured using only visible light. While many have demonstrated that SSL on medical images has resulted in better downstream task performance, our work suggests that more performance can be gained. The scientific principles which are used to acquire medical images are not often considered when constructing learning problems. For this reason, we propose incorporating quantitative imaging principles during generative SSL to improve image quality and quantitative biological accuracy. We show that this training schema results in better starting states for downstream supervised training on limited data. Our model also generates images that validate on clinical quantitative analysis software.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge