Jeremy Levy
Generalization in medical AI: a perspective on developing scalable models
Nov 09, 2023


Abstract:Over the past few years, research has witnessed the advancement of deep learning models trained on large datasets, some even encompassing millions of examples. While these impressive performance on their hidden test sets, they often underperform when assessed on external datasets. Recognizing the critical role of generalization in medical AI development, many prestigious journals now require reporting results both on the local hidden test set as well as on external datasets before considering a study for publication. Effectively, the field of medical AI has transitioned from the traditional usage of a single dataset that is split into train and test to a more comprehensive framework using multiple datasets, some of which are used for model development (source domain) and others for testing (target domains). However, this new experimental setting does not necessarily resolve the challenge of generalization. This is because of the variability encountered in intended use and specificities across hospital cultures making the idea of universally generalizable systems a myth. On the other hand, the systematic, and a fortiori recurrent re-calibration, of models at the individual hospital level, although ideal, may be overoptimistic given the legal, regulatory and technical challenges that are involved. Re-calibration using transfer learning may not even be possible in some instances where reference labels of target domains are not available. In this perspective we establish a hierarchical three-level scale system reflecting the generalization level of a medical AI algorithm. This scale better reflects the diversity of real-world medical scenarios per which target domain data for re-calibration of models may or not be available and if it is, may or not have reference labels systematically available.
Distortion measure of spectrograms for classification of respiratory diseases
Jun 04, 2021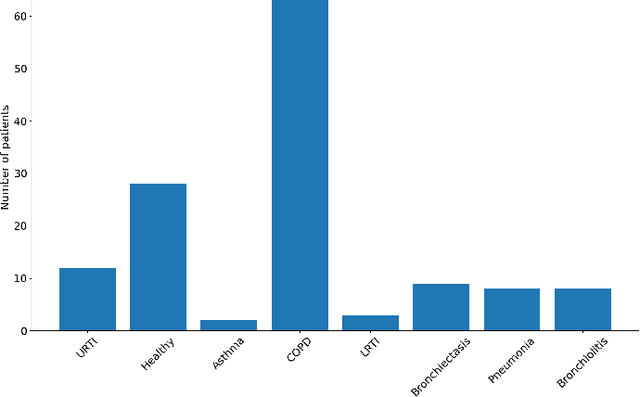
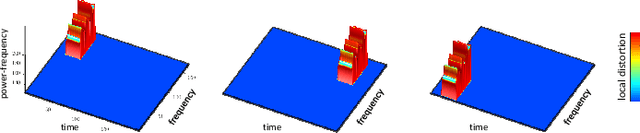
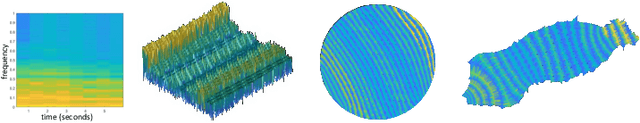
Abstract:A new method for the classification of respiratory diseases is presented. The method is based on a novel class of features, extracted from pulmonary sounds, by parameterizing their spectrograms that are represented as surfaces, and by utilizing geometrical distortions defined with reference to these surfaces. This method yields a set of highly descriptive features for the analysis of pulmonary sound recordings. Furthermore, by combining these features with Mel-frequency cepstral coefficients, we introduce a powerful model for the automatic diagnosis of common respiratory pathologies. Compared with baseline methods, our model achieves superior results for binary and multi-class classifications of common respiratory diseases. Our new approach to the classification of one-dimensional signals is applicable to other signals in the context of their representations in combined spaces or manifolds.
Machine learning for nocturnal diagnosis of chronic obstructive pulmonary disease using digital oximetry biomarkers
Dec 10, 2020



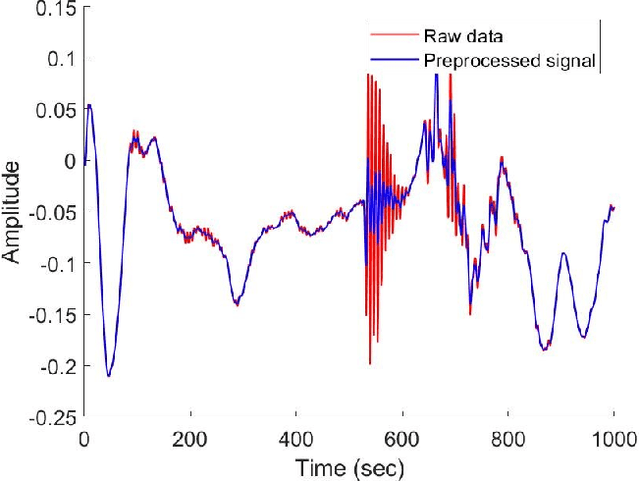
Abstract:Objective: Chronic obstructive pulmonary disease (COPD) is a highly prevalent chronic condition. COPD is a major source of morbidity, mortality and healthcare costs. Spirometry is the gold standard test for a definitive diagnosis and severity grading of COPD. However, a large proportion of individuals with COPD are undiagnosed and untreated. Given the high prevalence of COPD and its clinical importance, it is critical to develop new algorithms to identify undiagnosed COPD, especially in specific groups at risk, such as those with sleep disorder breathing. To our knowledge, no research has looked at the feasibility of COPD diagnosis from the nocturnal oximetry time series. Approach: We hypothesize that patients with COPD will exert certain patterns and/or dynamics of their overnight oximetry time series that are unique to this condition. We introduce a novel approach to nocturnal COPD diagnosis using 44 oximetry digital biomarkers and 5 demographic features and assess its performance in a population sample at risk of sleep-disordered breathing. A total of n=350 unique patients polysomnography (PSG) recordings. A random forest (RF) classifier is trained using these features and evaluated using the nested cross-validation procedure. Significance: Our research makes a number of novel scientific contributions. First, we demonstrated for the first time, the feasibility of COPD diagnosis from nocturnal oximetry time series in a population sample at risk of sleep disordered breathing. We highlighted what digital oximetry biomarkers best reflect how COPD manifests overnight. The results motivate that overnight single channel oximetry is a valuable pathway for COPD diagnosis.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge