Ethan Wu
Patient-Specific Models of Treatment Effects Explain Heterogeneity in Tuberculosis
Nov 16, 2024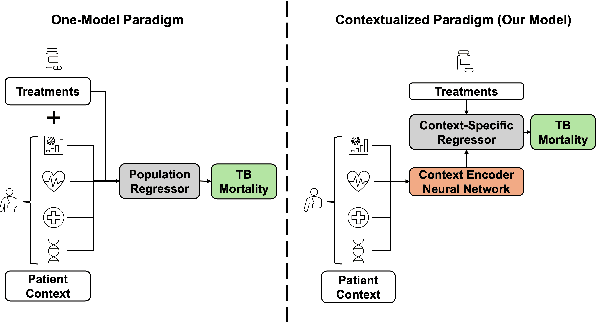
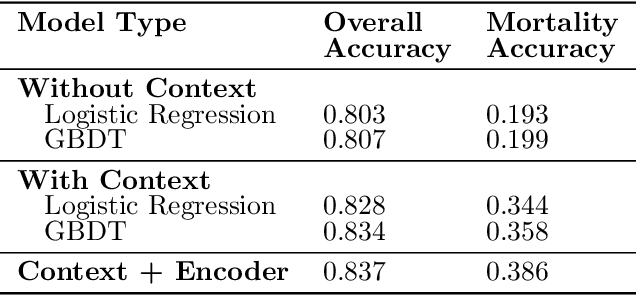
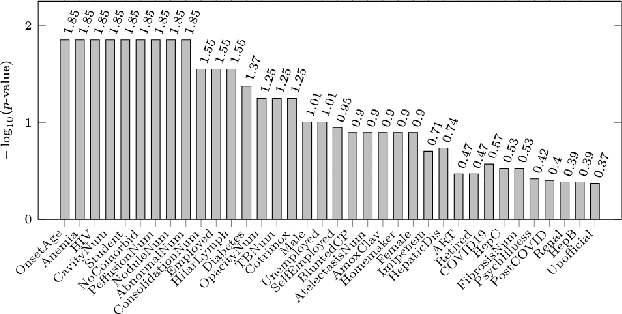
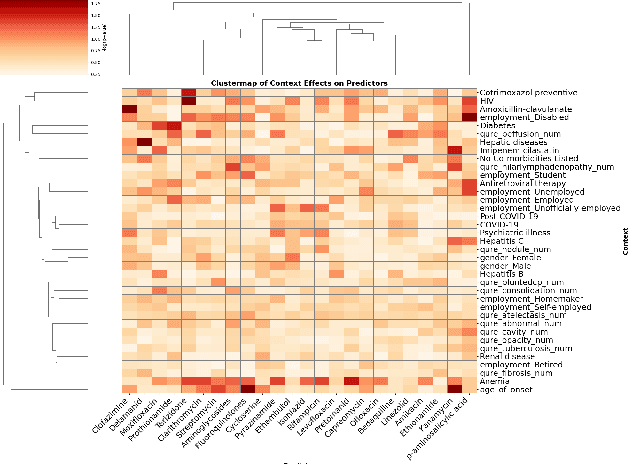
Abstract:Tuberculosis (TB) is a major global health challenge, and is compounded by co-morbidities such as HIV, diabetes, and anemia, which complicate treatment outcomes and contribute to heterogeneous patient responses. Traditional models of TB often overlook this heterogeneity by focusing on broad, pre-defined patient groups, thereby missing the nuanced effects of individual patient contexts. We propose moving beyond coarse subgroup analyses by using contextualized modeling, a multi-task learning approach that encodes patient context into personalized models of treatment effects, revealing patient-specific treatment benefits. Applied to the TB Portals dataset with multi-modal measurements for over 3,000 TB patients, our model reveals structured interactions between co-morbidities, treatments, and patient outcomes, identifying anemia, age of onset, and HIV as influential for treatment efficacy. By enhancing predictive accuracy in heterogeneous populations and providing patient-specific insights, contextualized models promise to enable new approaches to personalized treatment.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge