Alexandre Le Guilcher
Patch Progression Masked Autoencoder with Fusion CNN Network for Classifying Evolution Between Two Pairs of 2D OCT Slices
Aug 27, 2025Abstract:Age-related Macular Degeneration (AMD) is a prevalent eye condition affecting visual acuity. Anti-vascular endothelial growth factor (anti-VEGF) treatments have been effective in slowing the progression of neovascular AMD, with better outcomes achieved through timely diagnosis and consistent monitoring. Tracking the progression of neovascular activity in OCT scans of patients with exudative AMD allows for the development of more personalized and effective treatment plans. This was the focus of the Monitoring Age-related Macular Degeneration Progression in Optical Coherence Tomography (MARIO) challenge, in which we participated. In Task 1, which involved classifying the evolution between two pairs of 2D slices from consecutive OCT acquisitions, we employed a fusion CNN network with model ensembling to further enhance the model's performance. For Task 2, which focused on predicting progression over the next three months based on current exam data, we proposed the Patch Progression Masked Autoencoder that generates an OCT for the next exam and then classifies the evolution between the current OCT and the one generated using our solution from Task 1. The results we achieved allowed us to place in the Top 10 for both tasks. Some team members are part of the same organization as the challenge organizers; therefore, we are not eligible to compete for the prize.
* 10 pages, 5 figures, 3 tables, challenge/conference paper
Context-Aware Vision Language Foundation Models for Ocular Disease Screening in Retinal Images
Mar 19, 2025Abstract:Foundation models are large-scale versatile systems trained on vast quantities of diverse data to learn generalizable representations. Their adaptability with minimal fine-tuning makes them particularly promising for medical imaging, where data variability and domain shifts are major challenges. Currently, two types of foundation models dominate the literature: self-supervised models and more recent vision-language models. In this study, we advance the application of vision-language foundation (VLF) models for ocular disease screening using the OPHDIAT dataset, which includes nearly 700,000 fundus photographs from a French diabetic retinopathy (DR) screening network. This dataset provides extensive clinical data (patient-specific information such as diabetic health conditions, and treatments), labeled diagnostics, ophthalmologists text-based findings, and multiple retinal images for each examination. Building on the FLAIR model $\unicode{x2013}$ a VLF model for retinal pathology classification $\unicode{x2013}$ we propose novel context-aware VLF models (e.g jointly analyzing multiple images from the same visit or taking advantage of past diagnoses and contextual data) to fully leverage the richness of the OPHDIAT dataset and enhance robustness to domain shifts. Our approaches were evaluated on both in-domain (a testing subset of OPHDIAT) and out-of-domain data (public datasets) to assess their generalization performance. Our model demonstrated improved in-domain performance for DR grading, achieving an area under the curve (AUC) ranging from 0.851 to 0.9999, and generalized well to ocular disease detection on out-of-domain data (AUC: 0.631-0.913).
Generalizing deep learning models for medical image classification
Mar 21, 2024Abstract:Numerous Deep Learning (DL) models have been developed for a large spectrum of medical image analysis applications, which promises to reshape various facets of medical practice. Despite early advances in DL model validation and implementation, which encourage healthcare institutions to adopt them, some fundamental questions remain: are the DL models capable of generalizing? What causes a drop in DL model performances? How to overcome the DL model performance drop? Medical data are dynamic and prone to domain shift, due to multiple factors such as updates to medical equipment, new imaging workflow, and shifts in patient demographics or populations can induce this drift over time. In this paper, we review recent developments in generalization methods for DL-based classification models. We also discuss future challenges, including the need for improved evaluation protocols and benchmarks, and envisioned future developments to achieve robust, generalized models for medical image classification.
Instant automatic diagnosis of diabetic retinopathy
Jun 12, 2019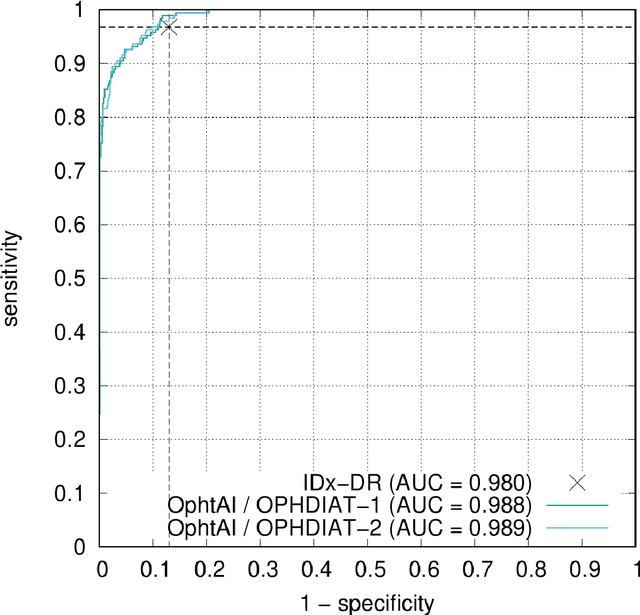
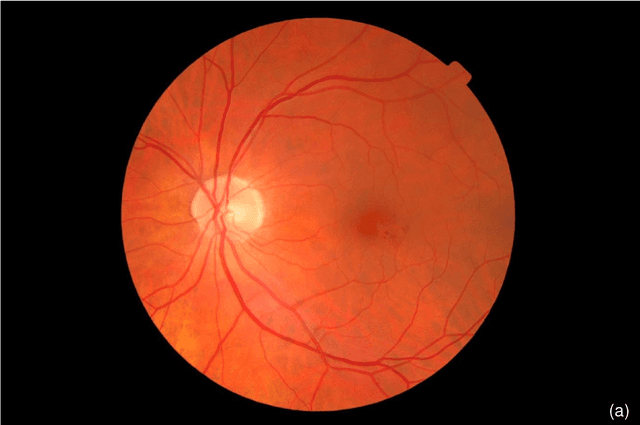
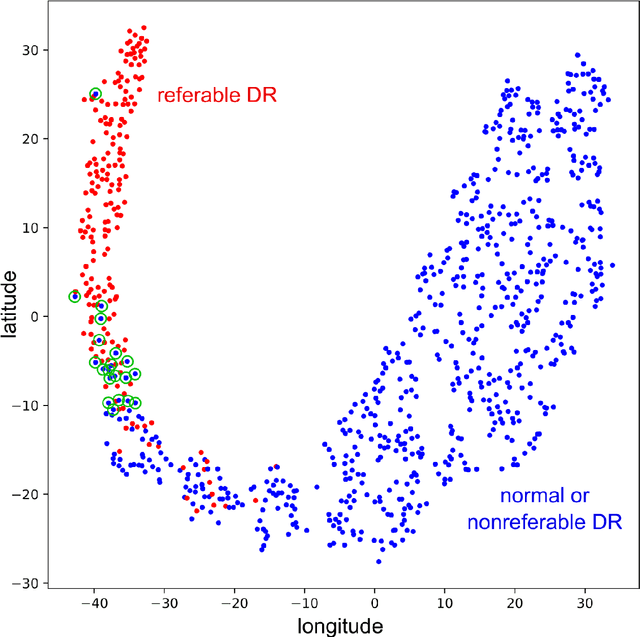
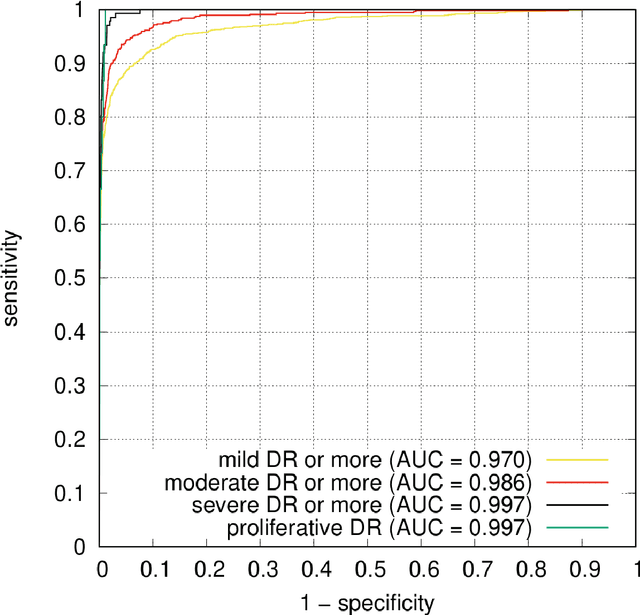
Abstract:The purpose of this study is to evaluate the performance of the OphtAI system for the automatic detection of referable diabetic retinopathy (DR) and the automatic assessment of DR severity using color fundus photography. OphtAI relies on ensembles of convolutional neural networks trained to recognize eye laterality, detect referable DR and assess DR severity. The system can either process single images or full examination records. To document the automatic diagnoses, accurate heatmaps are generated. The system was developed and validated using a dataset of 763,848 images from 164,660 screening procedures from the OPHDIAT screening program. For comparison purposes, it was also evaluated in the public Messidor-2 dataset. Referable DR can be detected with an area under the ROC curve of AUC = 0.989 in the Messidor-2 dataset, using the University of Iowa's reference standard (95% CI: 0.984-0.994). This is significantly better than the only AI system authorized by the FDA, evaluated in the exact same conditions (AUC = 0.980). OphtAI can also detect vision-threatening DR with an AUC of 0.997 (95% CI: 0.996-0.998) and proliferative DR with an AUC of 0.997 (95% CI: 0.995-0.999). The system runs in 0.3 seconds using a graphics processing unit and less than 2 seconds without. OphtAI is safer, faster and more comprehensive than the only AI system authorized by the FDA so far. Instant DR diagnosis is now possible, which is expected to streamline DR screening and to give easy access to DR screening to more diabetic patients.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge