Shawn Shadden
LinFlo-Net: A two-stage deep learning method to generate simulation ready meshes of the heart
Oct 30, 2023Abstract:We present a deep learning model to automatically generate computer models of the human heart from patient imaging data with an emphasis on its capability to generate thin-walled cardiac structures. Our method works by deforming a template mesh to fit the cardiac structures to the given image. Compared with prior deep learning methods that adopted this approach, our framework is designed to minimize mesh self-penetration, which typically arises when deforming surface meshes separated by small distances. We achieve this by using a two-stage diffeomorphic deformation process along with a novel loss function derived from the kinematics of motion that penalizes surface contact and interpenetration. Our model demonstrates comparable accuracy with state-of-the-art methods while additionally producing meshes free of self-intersections. The resultant meshes are readily usable in physics based simulation, minimizing the need for post-processing and cleanup.
Learning Whole Heart Mesh Generation From Patient Images For Computational Simulations
Mar 20, 2022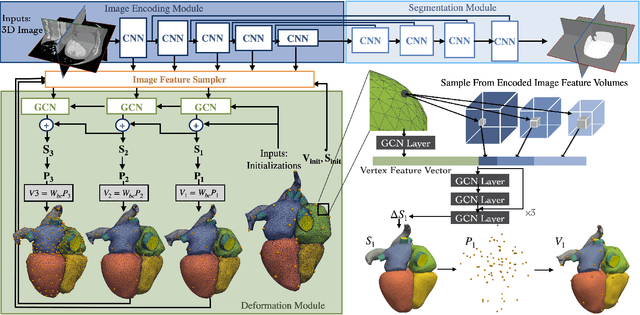
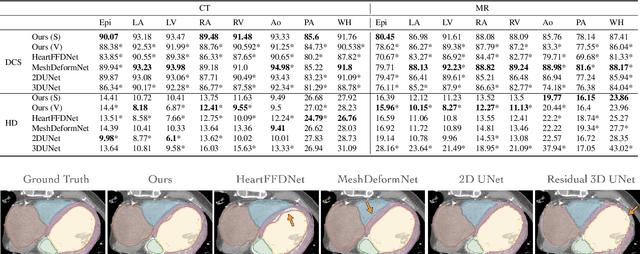
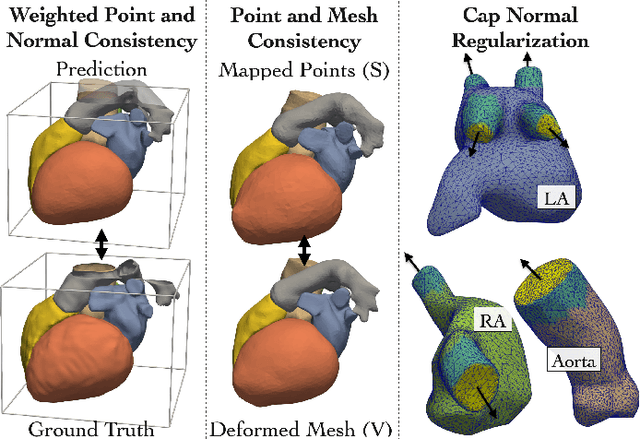
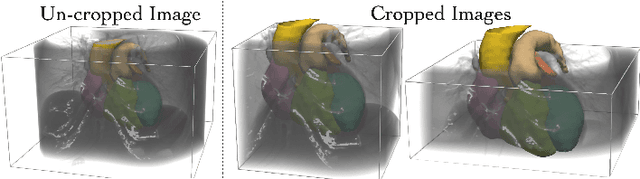
Abstract:Patient-specific cardiac modeling combines geometries of the heart derived from medical images and biophysical simulations to predict various aspects of cardiac function. However, generating simulation-suitable models of the heart from patient image data often requires complicated procedures and significant human effort. We present a fast and automated deep-learning method to construct simulation-suitable models of the heart from medical images. The approach constructs meshes from 3D patient images by learning to deform a small set of deformation handles on a whole heart template. For both 3D CT and MR data, this method achieves promising accuracy for whole heart reconstruction, consistently outperforming prior methods in constructing simulation-suitable meshes of the heart. When evaluated on time-series CT data, this method produced more anatomically and temporally consistent geometries than prior methods, and was able to produce geometries that better satisfy modeling requirements for cardiac flow simulations. Our source code will be available on GitHub.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge