Christopher Josef
DeepAISE -- An End-to-End Development and Deployment of a Recurrent Neural Survival Model for Early Prediction of Sepsis
Aug 10, 2019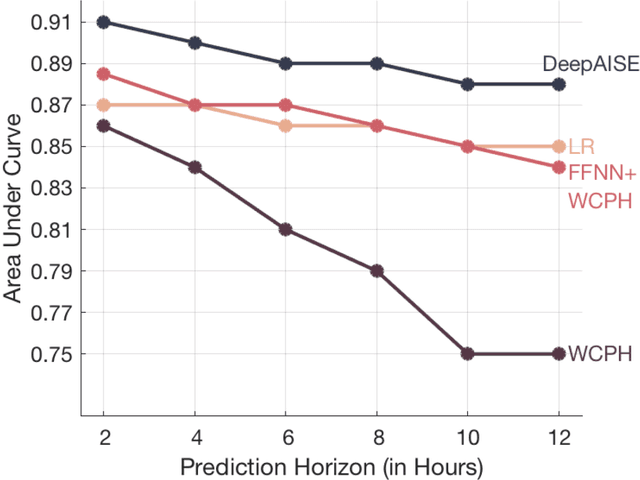
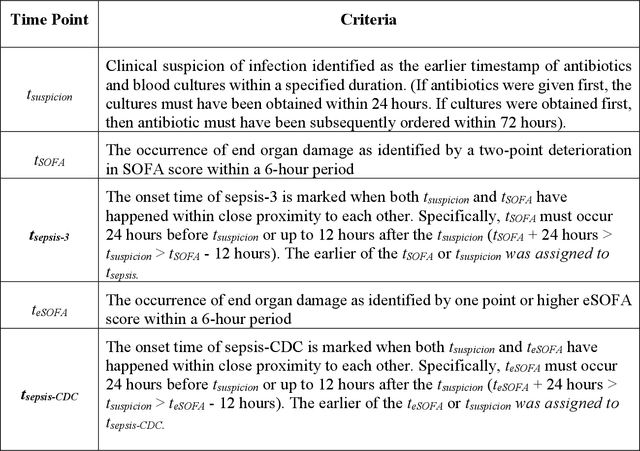
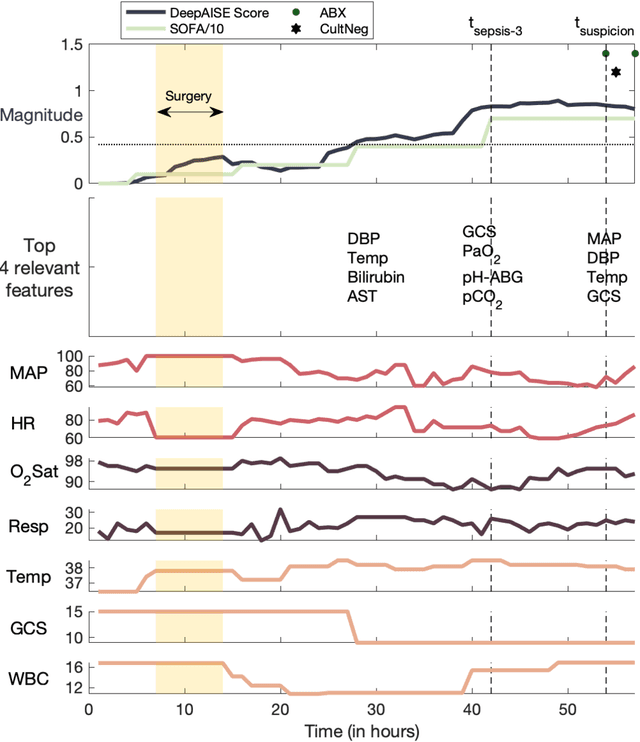
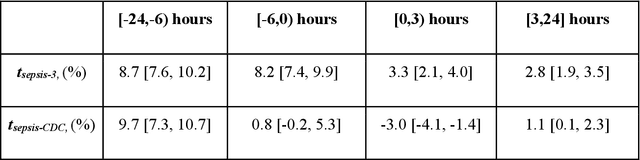
Abstract:Sepsis, a dysregulated immune system response to infection, is among the leading causes of morbidity, mortality, and cost overruns in the Intensive Care Unit (ICU). Early prediction of sepsis can improve situational awareness amongst clinicians and facilitate timely, protective interventions. While the application of predictive analytics in ICU patients has shown early promising results, much of the work has been encumbered by high false-alarm rates. Efforts to improve specificity have been limited by several factors, most notably the difficulty of labeling sepsis onset time and the low prevalence of septic-events in the ICU. Here, we present DeepAISE (Deep Artificial Intelligence Sepsis Expert), a recurrent neural survival model for the early prediction of sepsis. We show that by coupling a clinical criterion for defining sepsis onset time with a treatment policy (e.g., initiation of antibiotics within one hour of meeting the criterion), one may rank the relative utility of various criteria through offline policy evaluation. Given the optimal criterion, DeepAISE automatically learns predictive features related to higher-order interactions and temporal patterns among clinical risk factors that maximize the data likelihood of observed time to septic events. DeepAISE has been incorporated into a clinical workflow, which provides real-time hourly sepsis risk scores. A comparative study of four baseline models indicates that DeepAISE produces the most accurate predictions (AUC=0.90 and 0.87) and the lowest false alarm rates (FAR=0.20 and 0.26) in two separate cohorts (internal and external, respectively), while simultaneously producing interpretable representations of the clinical time series and risk factors.
Does the "Artificial Intelligence Clinician" learn optimal treatment strategies for sepsis in intensive care?
Feb 08, 2019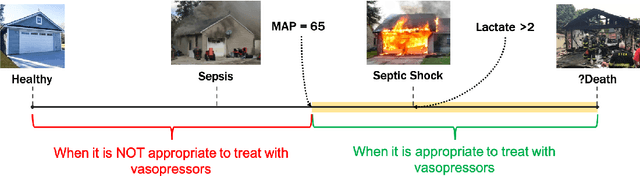
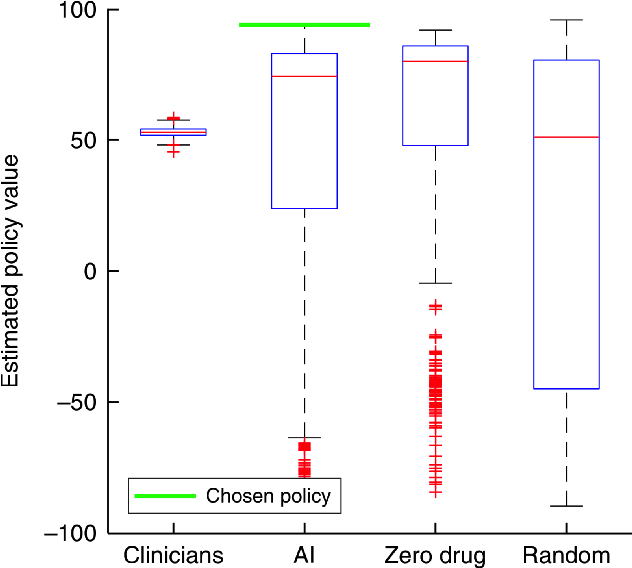
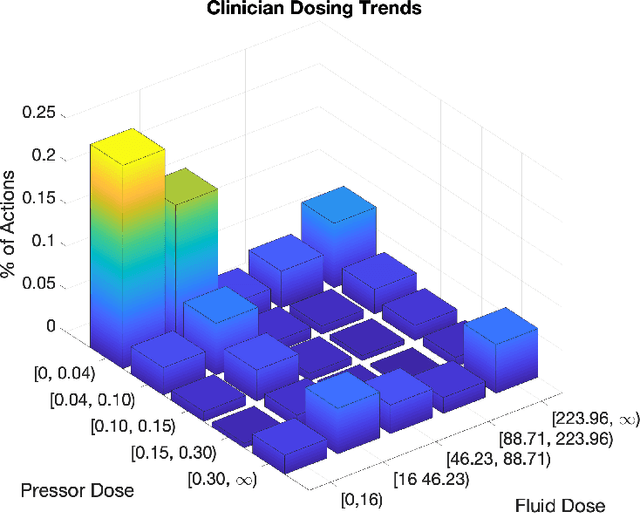
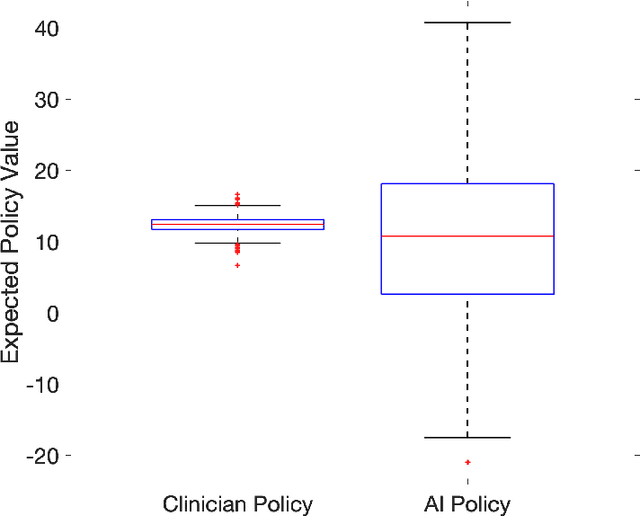
Abstract:From 2017 to 2018 the number of scientific publications found via PubMed search using the keyword "Machine Learning" increased by 46% (4,317 to 6,307). The results of studies involving machine learning, artificial intelligence (AI), and big data have captured the attention of healthcare practitioners, healthcare managers, and the public at a time when Western medicine grapples with unmitigated cost increases and public demands for accountability. The complexity involved in healthcare applications of machine learning and the size of the associated data sets has afforded many researchers an uncontested opportunity to satisfy these demands with relatively little oversight. In a recent Nature Medicine article, "The Artificial Intelligence Clinician learns optimal treatment strategies for sepsis in intensive care," Komorowski and his coauthors propose methods to train an artificial intelligence clinician to treat sepsis patients with vasopressors and IV fluids. In this post, we will closely examine the claims laid out in this paper. In particular, we will study the individual treatment profiles suggested by their AI Clinician to gain insight into how their AI Clinician intends to treat patients on an individual level.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge