Billy Wu
Fast and Generalizable parameter-embedded Neural Operators for Lithium-Ion Battery Simulation
Aug 11, 2025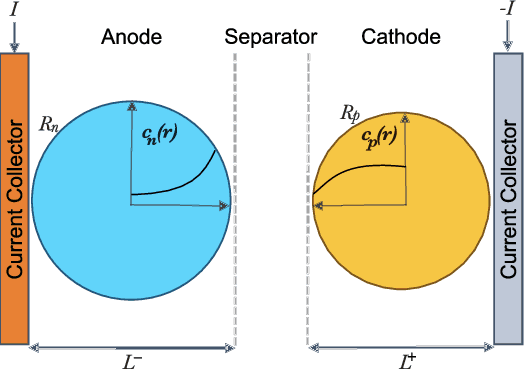
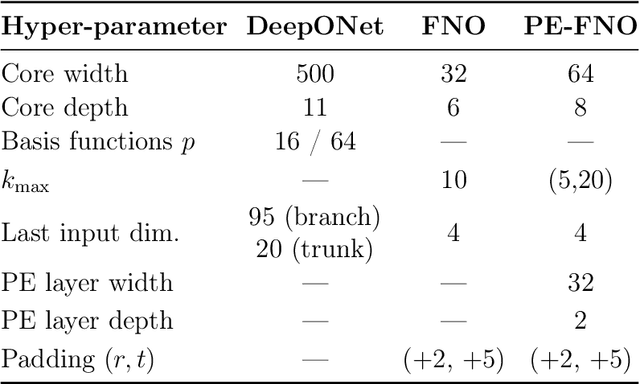
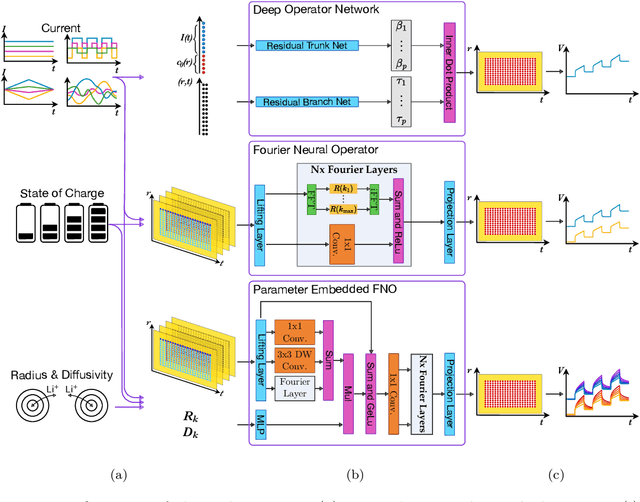
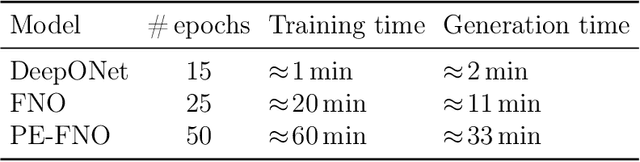
Abstract:Reliable digital twins of lithium-ion batteries must achieve high physical fidelity with sub-millisecond speed. In this work, we benchmark three operator-learning surrogates for the Single Particle Model (SPM): Deep Operator Networks (DeepONets), Fourier Neural Operators (FNOs) and a newly proposed parameter-embedded Fourier Neural Operator (PE-FNO), which conditions each spectral layer on particle radius and solid-phase diffusivity. Models are trained on simulated trajectories spanning four current families (constant, triangular, pulse-train, and Gaussian-random-field) and a full range of State-of-Charge (SOC) (0 % to 100 %). DeepONet accurately replicates constant-current behaviour but struggles with more dynamic loads. The basic FNO maintains mesh invariance and keeps concentration errors below 1 %, with voltage mean-absolute errors under 1.7 mV across all load types. Introducing parameter embedding marginally increases error, but enables generalisation to varying radii and diffusivities. PE-FNO executes approximately 200 times faster than a 16-thread SPM solver. Consequently, PE-FNO's capabilities in inverse tasks are explored in a parameter estimation task with Bayesian optimisation, recovering anode and cathode diffusivities with 1.14 % and 8.4 % mean absolute percentage error, respectively, and 0.5918 percentage points higher error in comparison with classical methods. These results pave the way for neural operators to meet the accuracy, speed and parametric flexibility demands of real-time battery management, design-of-experiments and large-scale inference. PE-FNO outperforms conventional neural surrogates, offering a practical path towards high-speed and high-fidelity electrochemical digital twins.
Predicting cardiovascular risk from national administrative databases using a combined survival analysis and deep learning approach
Nov 28, 2020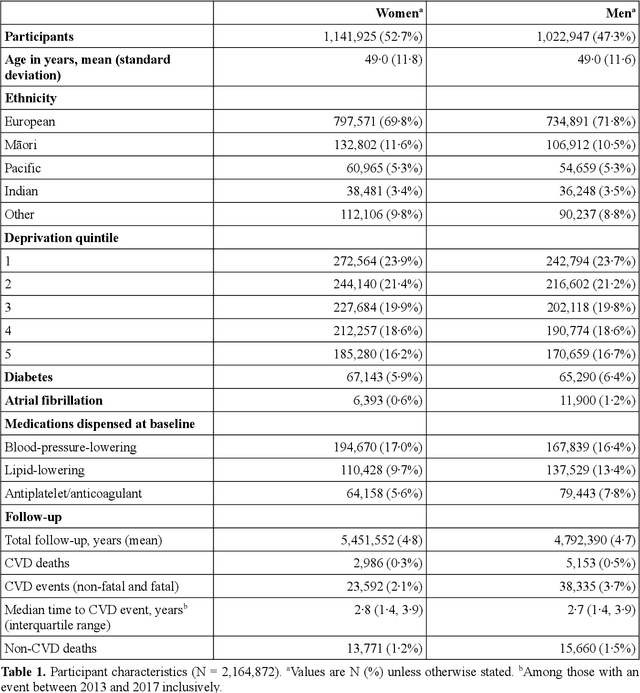
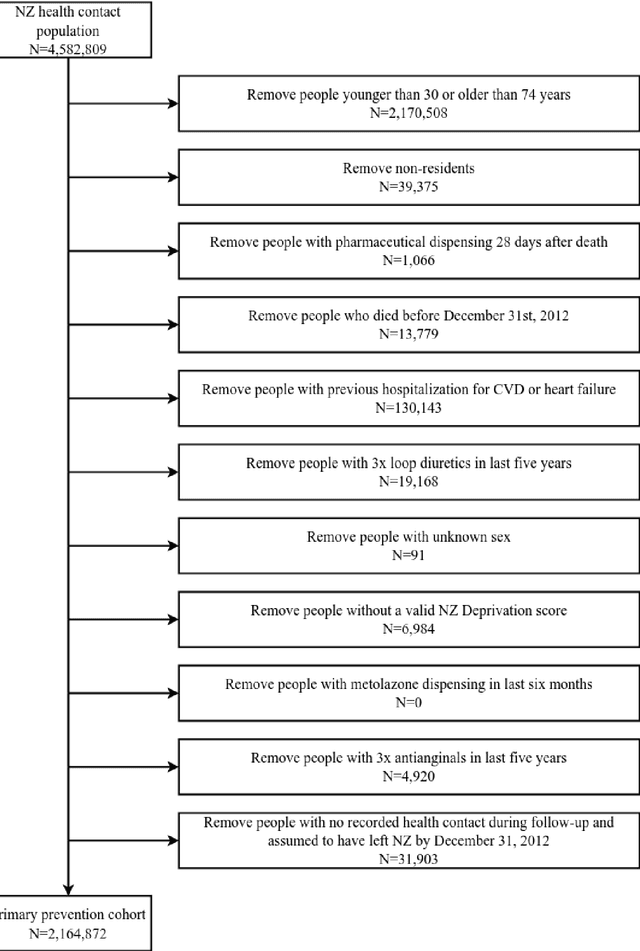
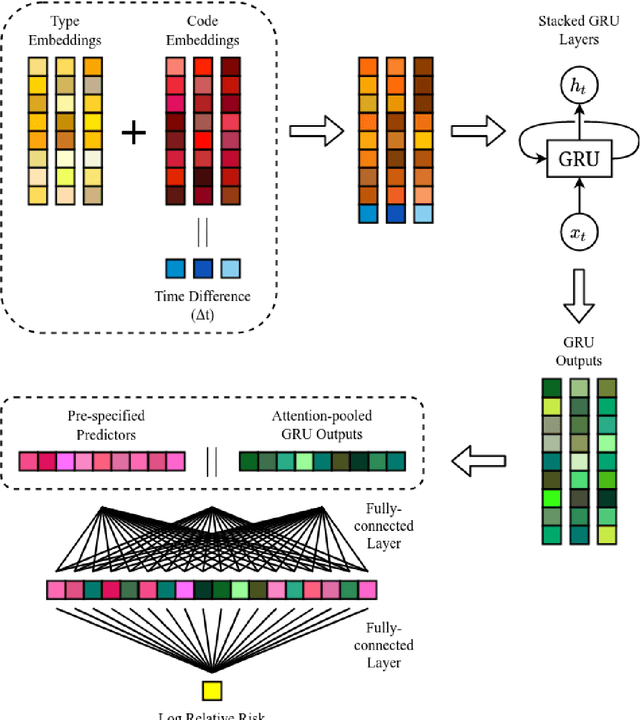
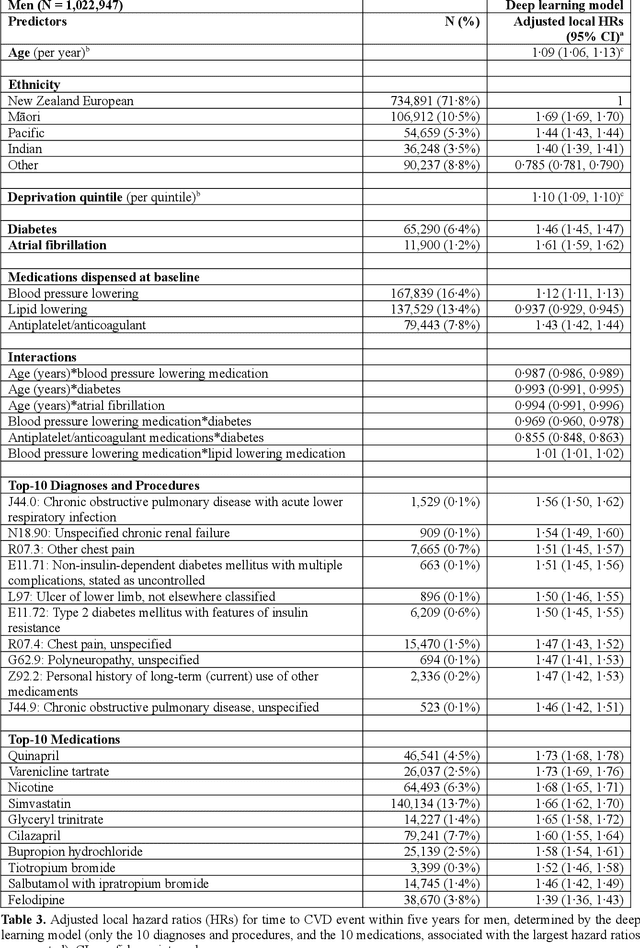
Abstract:AIMS. This study compared the performance of deep learning extensions of survival analysis models with traditional Cox proportional hazards (CPH) models for deriving cardiovascular disease (CVD) risk prediction equations in national health administrative datasets. METHODS. Using individual person linkage of multiple administrative datasets, we constructed a cohort of all New Zealand residents aged 30-74 years who interacted with publicly funded health services during 2012, and identified hospitalisations and deaths from CVD over five years of follow-up. After excluding people with prior CVD or heart failure, sex-specific deep learning and CPH models were developed to estimate the risk of fatal or non-fatal CVD events within five years. The proportion of explained time-to-event occurrence, calibration, and discrimination were compared between models across the whole study population and in specific risk groups. FINDINGS. First CVD events occurred in 61,927 of 2,164,872 people. Among diagnoses and procedures, the largest 'local' hazard ratios were associated by the deep learning models with tobacco use in women (2.04, 95%CI: 1.99-2.10) and with chronic obstructive pulmonary disease with acute lower respiratory infection in men (1.56, 95%CI: 1.50-1.62). Other identified predictors (e.g. hypertension, chest pain, diabetes) aligned with current knowledge about CVD risk predictors. The deep learning models significantly outperformed the CPH models on the basis of proportion of explained time-to-event occurrence (Royston and Sauerbrei's R-squared: 0.468 vs. 0.425 in women and 0.383 vs. 0.348 in men), calibration, and discrimination (all p<0.0001). INTERPRETATION. Deep learning extensions of survival analysis models can be applied to large health administrative databases to derive interpretable CVD risk prediction equations that are more accurate than traditional CPH models.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge