Audrey Duran
MYRIAD
ProstAttention-Net: A deep attention model for prostate cancer segmentation by aggressiveness in MRI scans
Nov 23, 2022



Abstract:Multiparametric magnetic resonance imaging (mp-MRI) has shown excellent results in the detection of prostate cancer (PCa). However, characterizing prostate lesions aggressiveness in mp-MRI sequences is impossible in clinical practice, and biopsy remains the reference to determine the Gleason score (GS). In this work, we propose a novel end-to-end multi-class network that jointly segments the prostate gland and cancer lesions with GS group grading. After encoding the information on a latent space, the network is separated in two branches: 1) the first branch performs prostate segmentation 2) the second branch uses this zonal prior as an attention gate for the detection and grading of prostate lesions. The model was trained and validated with a 5-fold cross-validation on an heterogeneous series of 219 MRI exams acquired on three different scanners prior prostatectomy. In the free-response receiver operating characteristics (FROC) analysis for clinically significant lesions (defined as GS > 6) detection, our model achieves 69.0% $\pm$14.5% sensitivity at 2.9 false positive per patient on the whole prostate and 70.8% $\pm$14.4% sensitivity at 1.5 false positive when considering the peripheral zone (PZ) only. Regarding the automatic GS group
Perfusion imaging in deep prostate cancer detection from mp-MRI: can we take advantage of it?
Jul 06, 2022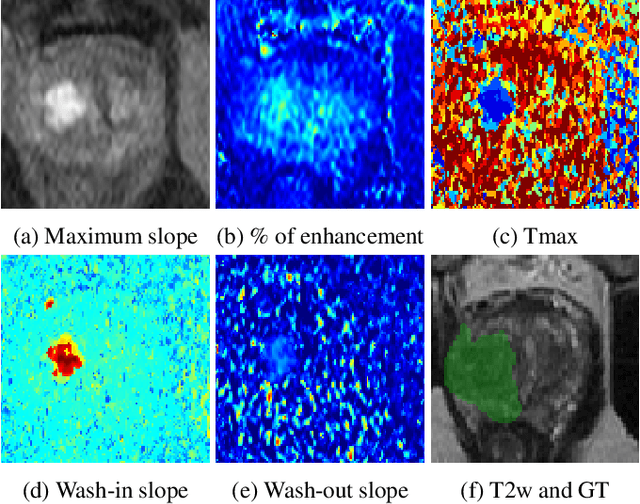

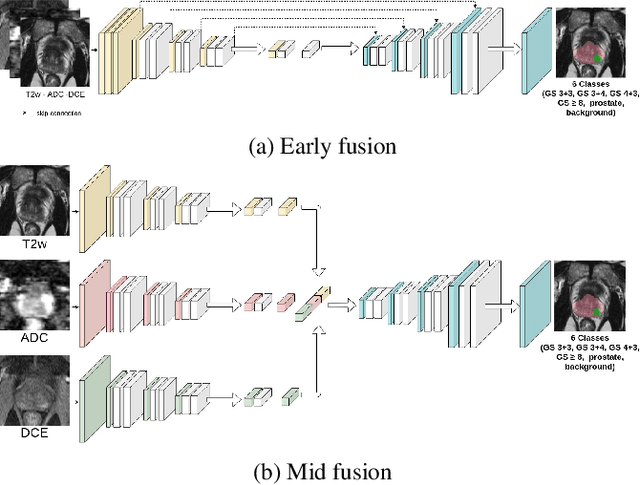

Abstract:To our knowledge, all deep computer-aided detection and diagnosis (CAD) systems for prostate cancer (PCa) detection consider bi-parametric magnetic resonance imaging (bp-MRI) only, including T2w and ADC sequences while excluding the 4D perfusion sequence,which is however part of standard clinical protocols for this diagnostic task. In this paper, we question strategies to integrate information from perfusion imaging in deep neural architectures. To do so, we evaluate several ways to encode the perfusion information in a U-Net like architecture, also considering early versus mid fusion strategies. We compare performance of multiparametric MRI (mp-MRI) models with the baseline bp-MRI model based on a private dataset of 219 mp-MRI exams. Perfusion maps derived from dynamic contrast enhanced MR exams are shown to positively impact segmentation and grading performance of PCa lesions, especially the 3D MR volume corresponding to the maximum slope of the wash-in curve as well as Tmax perfusion maps. The latter mp-MRI models indeed outperform the bp-MRI one whatever the fusion strategy, with Cohen's kappa score of 0.318$\pm$0.019 for the bp-MRI model and 0.378 $\pm$ 0.033 for the model including the maximum slope with a mid fusion strategy, also achieving competitive Cohen's kappa score compared to state of the art.
Learning to segment prostate cancer by aggressiveness from scribbles in bi-parametric MRI
Jul 01, 2022Abstract:In this work, we propose a deep U-Net based model to tackle the challenging task of prostate cancer segmentation by aggressiveness in MRI based on weak scribble annotations. This model extends the size constraint loss proposed by Kervadec et al. 1 in the context of multiclass detection and segmentation task. This model is of high clinical interest as it allows training on prostate biopsy samples and avoids time-consuming full annotation process. Performance is assessed on a private dataset (219 patients) where the full ground truth is available as well as on the ProstateX-2 challenge database, where only biopsy results at different localisations serve as reference. We show that we can approach the fully-supervised baseline in grading the lesions by using only 6.35% of voxels for training. We report a lesion-wise Cohen's kappa score of 0.29 $\pm$ 0.07 for the weak model versus 0.32 $\pm$ 0.05 for the baseline. We also report a kappa score (0.276 $\pm$ 0.037) on the ProstateX-2 challenge dataset with our weak U-Net trained on a combination of ProstateX-2 and our dataset, which is the highest reported value on this challenge dataset for a segmentation task to our knowledge.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge