Deterioration Prediction using Time-Series of Three Vital Signs and Current Clinical Features Amongst COVID-19 Patients
Paper and Code
Oct 12, 2022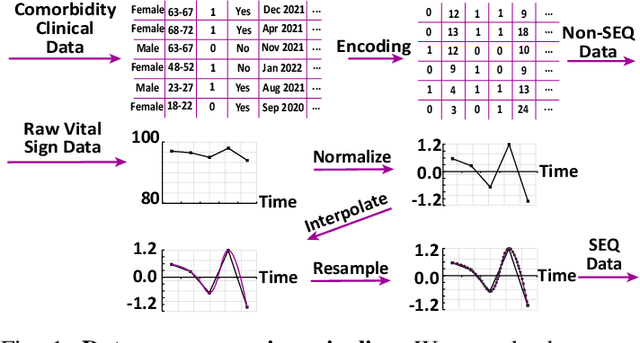
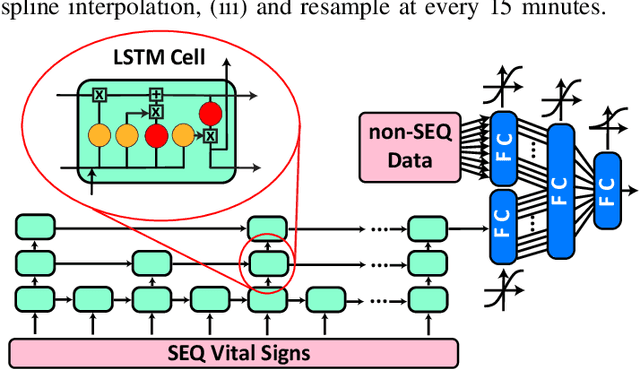
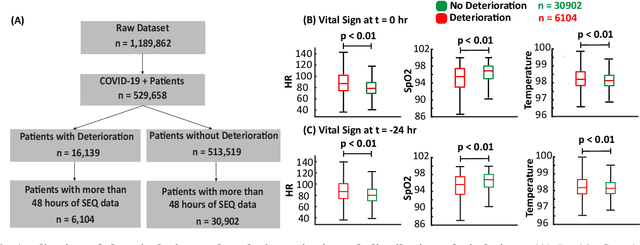
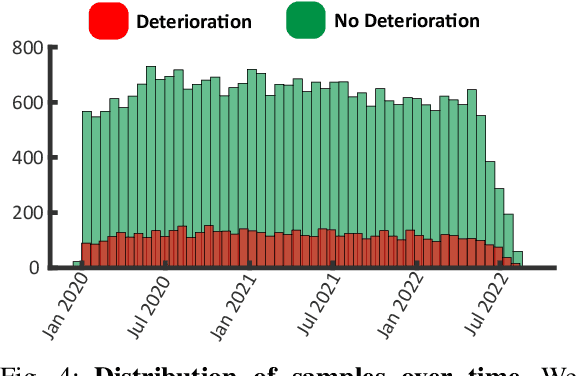
Unrecognized patient deterioration can lead to high morbidity and mortality. Most existing deterioration prediction models require a large number of clinical information, typically collected in hospital settings, such as medical images or comprehensive laboratory tests. This is infeasible for telehealth solutions and highlights a gap in deterioration prediction models that are based on minimal data, which can be recorded at a large scale in any clinic, nursing home, or even at the patient's home. In this study, we propose and develop a prognostic model that predicts if a patient will experience deterioration in the forthcoming 3-24 hours. The model sequentially processes routine triadic vital signs: (a) oxygen saturation, (b) heart rate, and (c) temperature. The model is also provided with basic patient information, including sex, age, vaccination status, vaccination date, and status of obesity, hypertension, or diabetes. We train and evaluate the model using data collected from 37,006 COVID-19 patients at NYU Langone Health in New York, USA. The model achieves an area under the receiver operating characteristic curve (AUROC) of 0.808-0.880 for 3-24 hour deterioration prediction. We also conduct occlusion experiments to evaluate the importance of each input feature, where the results reveal the significance of continuously monitoring the variations of the vital signs. Our results show the prospect of accurate deterioration forecast using a minimum feature set that can be relatively easily obtained using wearable devices and self-reported patient information.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge