Applying Artificial Intelligence to Clinical Decision Support in Mental Health: What Have We Learned?
Paper and Code
Mar 06, 2023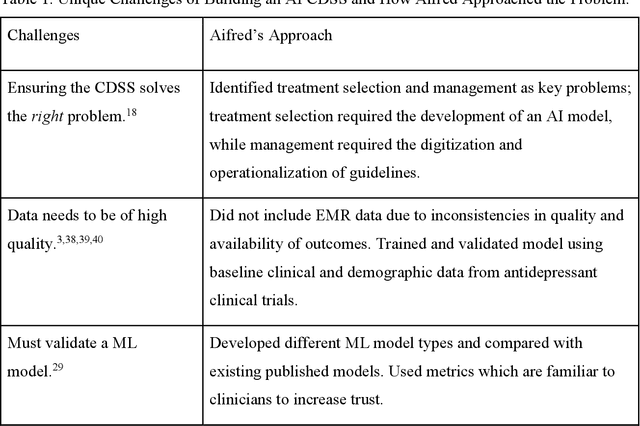
Clinical decision support systems (CDSS) augmented with artificial intelligence (AI) models are emerging as potentially valuable tools in healthcare. Despite their promise, the development and implementation of these systems typically encounter several barriers, hindering the potential for widespread adoption. Here we present a case study of a recently developed AI-CDSS, Aifred Health, aimed at supporting the selection and management of treatment in major depressive disorder. We consider both the principles espoused during development and testing of this AI-CDSS, as well as the practical solutions developed to facilitate implementation. We also propose recommendations to consider throughout the building, validation, training, and implementation process of an AI-CDSS. These recommendations include: identifying the key problem, selecting the type of machine learning approach based on this problem, determining the type of data required, determining the format required for a CDSS to provide clinical utility, gathering physician and patient feedback, and validating the tool across multiple settings. Finally, we explore the potential benefits of widespread adoption of these systems, while balancing these against implementation challenges such as ensuring systems do not disrupt the clinical workflow, and designing systems in a manner that engenders trust on the part of end users.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge