Nur Ahmad Khatim
Optimized Human-Robot Co-Dispatch Planning for Petro-Site Surveillance under Varying Criticalities
Feb 08, 2026Abstract:Securing petroleum infrastructure requires balancing autonomous system efficiency with human judgment for threat escalation, a challenge unaddressed by classical facility location models assuming homogeneous resources. This paper formulates the Human-Robot Co-Dispatch Facility Location Problem (HRCD-FLP), a capacitated facility location variant incorporating tiered infrastructure criticality, human-robot supervision ratio constraints, and minimum utilization requirements. We evaluate command center selection across three technology maturity scenarios. Results show transitioning from conservative (1:3 human-robot supervision) to future autonomous operations (1:10) yields significant cost reduction while maintaining complete critical infrastructure coverage. For small problems, exact methods dominate in both cost and computation time; for larger problems, the proposed heuristic achieves feasible solutions in under 3 minutes with approximately 14% optimality gap where comparison is possible. From systems perspective, our work demonstrate that optimized planning for human-robot teaming is key to achieve both cost-effective and mission-reliable deployments.
Using LLM for Real-Time Transcription and Summarization of Doctor-Patient Interactions into ePuskesmas in Indonesia
Sep 25, 2024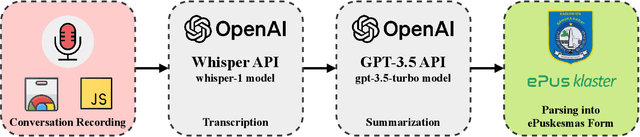
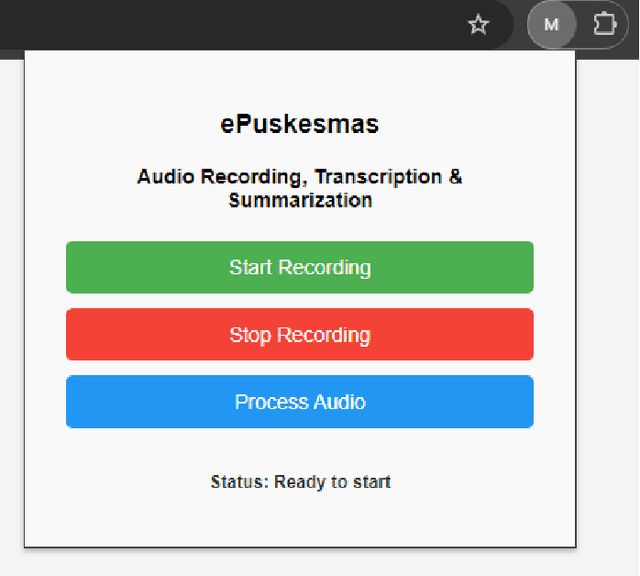
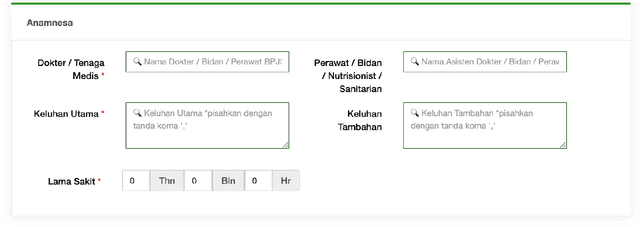
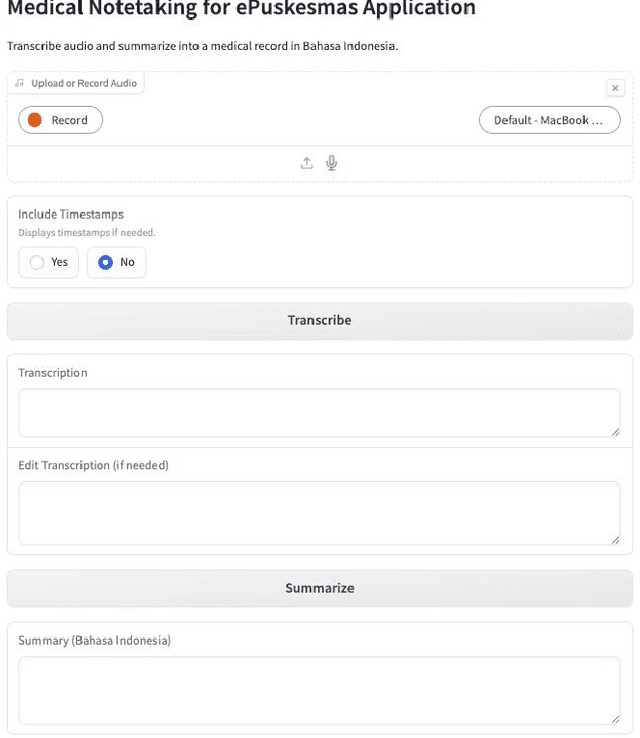
Abstract:One of the key issues contributing to inefficiency in Puskesmas is the time-consuming nature of doctor-patient interactions. Doctors need to conduct thorough consultations, which include diagnosing the patient's condition, providing treatment advice, and transcribing detailed notes into medical records. In regions with diverse linguistic backgrounds, doctors often have to ask clarifying questions, further prolonging the process. While diagnosing is essential, transcription and summarization can often be automated using AI to improve time efficiency and help doctors enhance care quality and enable early diagnosis and intervention. This paper proposes a solution using a localized large language model (LLM) to transcribe, translate, and summarize doctor-patient conversations. We utilize the Whisper model for transcription and GPT-3 to summarize them into the ePuskemas medical records format. This system is implemented as an add-on to an existing web browser extension, allowing doctors to fill out patient forms while talking. By leveraging this solution for real-time transcription, translation, and summarization, doctors can improve the turnaround time for patient care while enhancing the quality of records, which become more detailed and insightful for future visits. This innovation addresses challenges like overcrowded facilities and the administrative burden on healthcare providers in Indonesia. We believe this solution will help doctors save time, provide better care, and produce more accurate medical records, representing a significant step toward modernizing healthcare and ensuring patients receive timely, high-quality care, even in resource-constrained settings.
Toward an Integrated Decision Making Framework for Optimized Stroke Diagnosis with DSA and Treatment under Uncertainty
Jul 24, 2024Abstract:This study addresses the challenge of stroke diagnosis and treatment under uncertainty, a critical issue given the rapid progression and severe consequences of stroke conditions such as aneurysms, arteriovenous malformations (AVM), and occlusions. Current diagnostic methods, including Digital Subtraction Angiography (DSA), face limitations due to high costs and its invasive nature. To overcome these challenges, we propose a novel approach using a Partially Observable Markov Decision Process (POMDP) framework. Our model integrates advanced diagnostic tools and treatment approaches with a decision-making algorithm that accounts for the inherent uncertainties in stroke diagnosis. Our approach combines noisy observations from CT scans, Siriraj scores, and DSA reports to inform the subsequent treatment options. We utilize the online solver DESPOT, which employs tree-search methods and particle filters, to simulate potential future scenarios and guide our strategies. The results indicate that our POMDP framework balances diagnostic and treatment objectives, striking a tradeoff between the need for precise stroke identification via invasive procedures like DSA and the constraints of limited healthcare resources that necessitate more cost-effective strategies, such as in-hospital or at-home observation, by relying only relying on simulation rollouts and not imposing any prior knowledge. Our study offers a significant contribution by presenting a systematic framework that optimally integrates diagnostic and treatment processes for stroke and accounting for various uncertainties, thereby improving care and outcomes in stroke management.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge