Nicolai Ladegaard
Real-time unobtrusive sleep monitoring of in-patients with affective disorders: a feasibility study
Nov 22, 2023
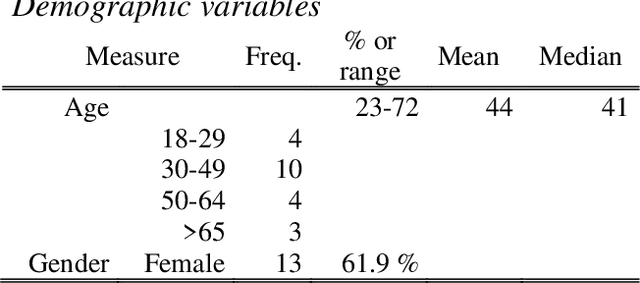
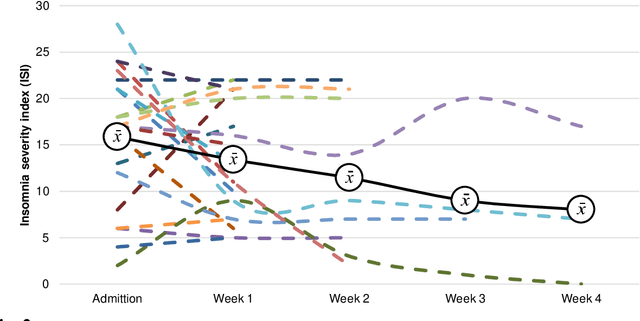
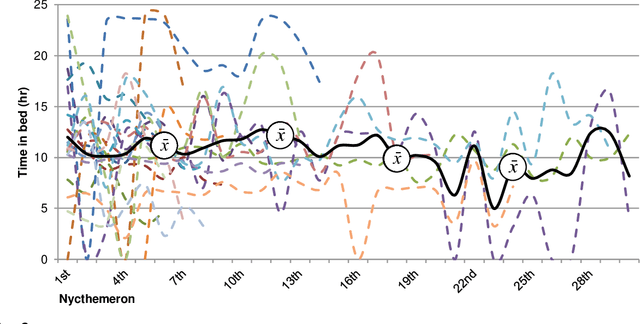
Abstract:Sleep and mental health are highly related concepts, and it is an important research and clinical priority to understand their interactions. In-bed sensors using ballistocardiography provide the possibility of unobtrusive measurements of sleep. In this study, we examined the feasibility of ballistocardiography in measuring key aspects of sleep in psychiatric in-patients. Specifically, we examined a sample of patients diagnosed with depression and bipolar disorder. The subjective experiences of the researchers conducting the study are explored and descriptive analyses of patient sleep are subsequently presented. The practicalities of using the ballistocardiography device seem to be favourable. There were no apparent issues regarding data quality or data integrity. Of clinical interest, we found no link between length of stay and reduced time in bed (b = -0.06, SE = 0.03, t = -1.76, p = .08). Using ballistocardiography for measurements on in-patients with affective disorders seems to be a feasible approach.
Automated speech- and text-based classification of neuropsychiatric conditions in a multidiagnostic setting
Jan 13, 2023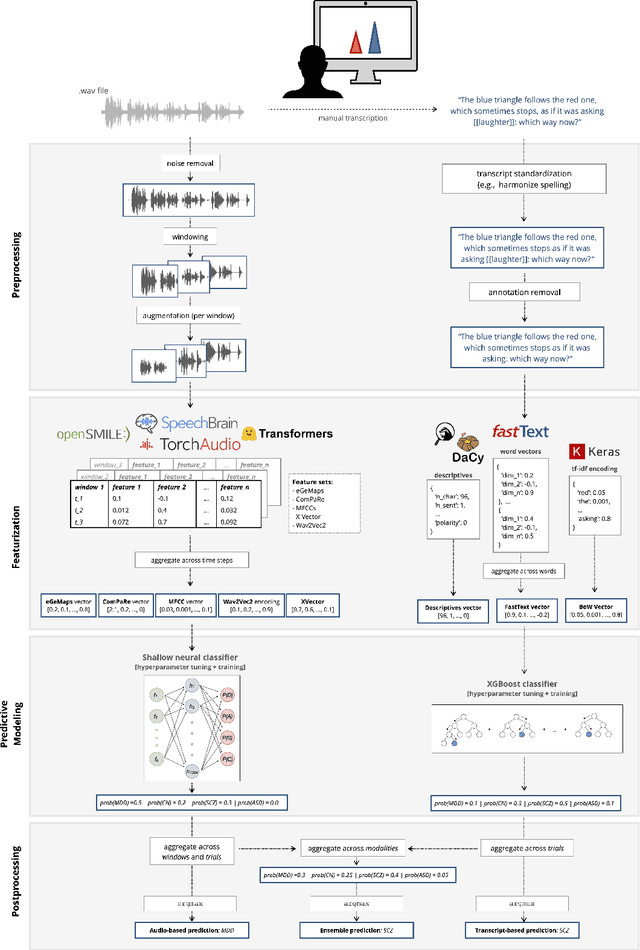
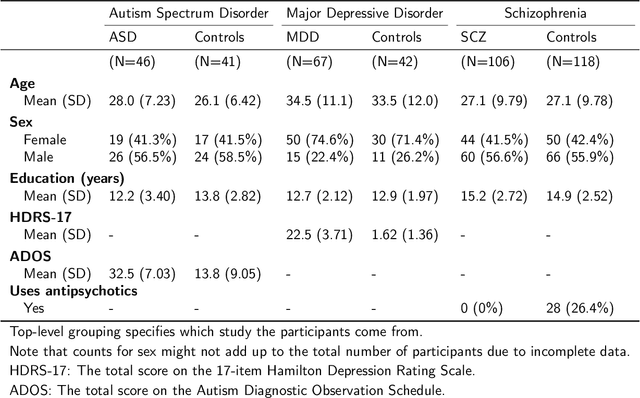
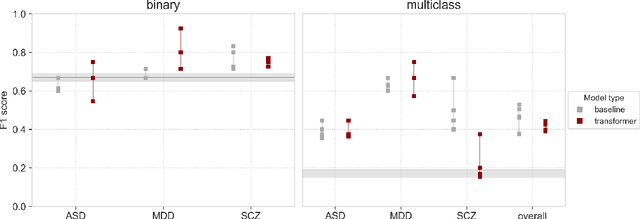
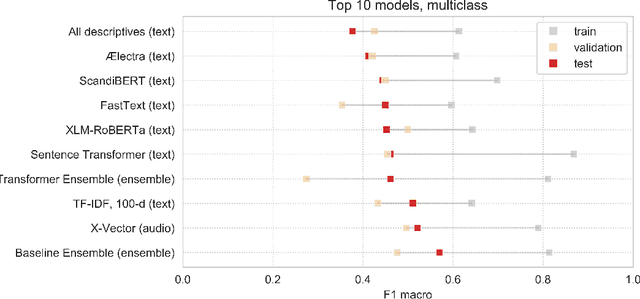
Abstract:Speech patterns have been identified as potential diagnostic markers for neuropsychiatric conditions. However, most studies only compare a single clinical group to healthy controls, whereas clinical practice often requires differentiating between multiple potential diagnoses (multiclass settings). To address this, we assembled a dataset of repeated recordings from 420 participants (67 with major depressive disorder, 106 with schizophrenia and 46 with autism, as well as matched controls), and tested the performance of a range of conventional machine learning models and advanced Transformer models on both binary and multiclass classification, based on voice and text features. While binary models performed comparably to previous research (F1 scores between 0.54-0.75 for autism spectrum disorder, ASD; 0.67-0.92 for major depressive disorder, MDD; and 0.71-0.83 for schizophrenia); when differentiating between multiple diagnostic groups performance decreased markedly (F1 scores between 0.35-0.44 for ASD, 0.57-0.75 for MDD, 0.15-0.66 for schizophrenia, and 0.38-0.52 macro F1). Combining voice and text-based models yielded increased performance, suggesting that they capture complementary diagnostic information. Our results indicate that models trained on binary classification may learn to rely on markers of generic differences between clinical and non-clinical populations, or markers of clinical features that overlap across conditions, rather than identifying markers specific to individual conditions. We provide recommendations for future research in the field, suggesting increased focus on developing larger transdiagnostic datasets that include more fine-grained clinical features, and that can support the development of models that better capture the complexity of neuropsychiatric conditions and naturalistic diagnostic assessment.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge