Farhad Piri
The automatic detection of lumber anatomy in epidural injections for ultrasound guidance
Dec 07, 2023Abstract:The purpose of this paper is to help the anesthesiologist to find the epidural depth automatically to make the first attempt to enter the path of the needle into the patient's body while it is clogged with bone and avoid causing a puncture in the surrounding areas of the patient`s back. In this regard, a morphology-based bone enhancement and detection followed by a Ramer-Douglas-Peucker algorithm and Hough transform is proposed. The proposed algorithm is tested on synthetic and real ultrasound images of laminar bone, and the results are compared with the template matching based Ligamentum Flavum (LF) detection method. Results indicate that the proposed method can faster detect the diagonal shape of the laminar bone and its corresponding epidural depth. Furthermore, the proposed method is reliable enough providing anesthesiologists with real-time information while an epidural needle insertion is performed. It has to be noted that using the ultrasound images is to help anesthesiologists to perform the blind injection, and due to quite a lot of errors occurred in ultrasound-imaging-based methods, these methods can not completely replace the tissue pressure-based method. And in the end, when the needle is injected into the area (dura space) measurements can only be trusted to the extent of tissue resistance. Despite the fairly limited amount of training data available in this study, a significant improvement of the segmentation speed of lumbar bones and epidural depth in ultrasound scans with a rational accuracy compared to the LF-based detection method was found.
End-to-End assessment of AR-assisted neurosurgery systems
Nov 03, 2023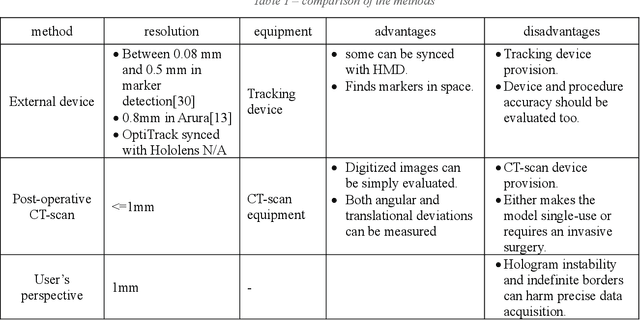
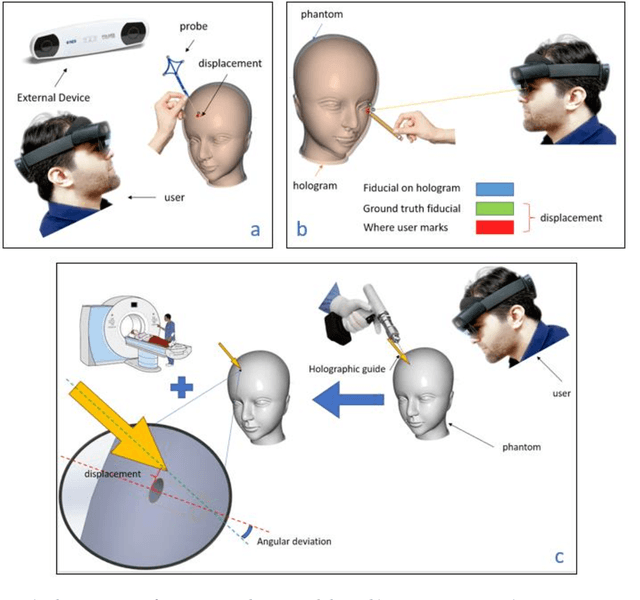
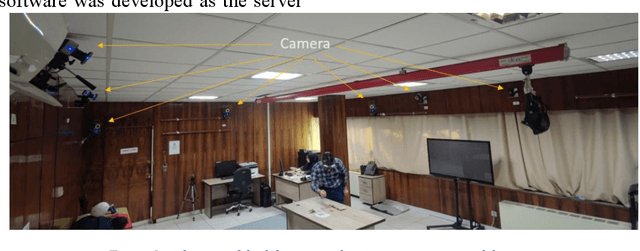
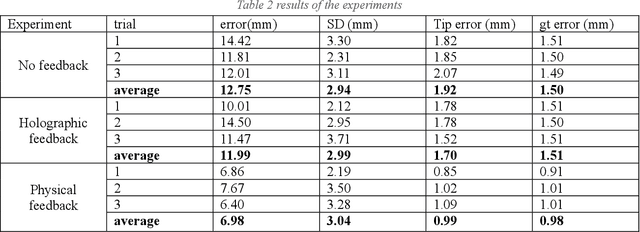
Abstract:Augmented Reality (AR) has emerged as a significant advancement in surgical procedures, offering a solution to the challenges posed by traditional neuronavigation methods. These conventional techniques often necessitate surgeons to split their focus between the surgical site and a separate monitor that displays guiding images. Over the years, many systems have been developed to register and track the hologram at the targeted locations, each employed its own evaluation technique. On the other hand, hologram displacement measurement is not a straightforward task because of various factors such as occlusion, Vengence-Accomodation Conflict, and unstable holograms in space. In this study, we explore and classify different techniques for assessing an AR-assisted neurosurgery system and propose a new technique to systematize the assessment procedure. Moreover, we conduct a deeper investigation to assess surgeon error in the pre- and intra-operative phases of the surgery based on the respective feedback given. We found that although the system can undergo registration and tracking errors, physical feedback can significantly reduce the error caused by hologram displacement. However, the lack of visual feedback on the hologram does not have a significant effect on the user 3D perception.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge