Donghao Qiao
CoBEVFusion: Cooperative Perception with LiDAR-Camera Bird's-Eye View Fusion
Oct 09, 2023Abstract:Autonomous Vehicles (AVs) use multiple sensors to gather information about their surroundings. By sharing sensor data between Connected Autonomous Vehicles (CAVs), the safety and reliability of these vehicles can be improved through a concept known as cooperative perception. However, recent approaches in cooperative perception only share single sensor information such as cameras or LiDAR. In this research, we explore the fusion of multiple sensor data sources and present a framework, called CoBEVFusion, that fuses LiDAR and camera data to create a Bird's-Eye View (BEV) representation. The CAVs process the multi-modal data locally and utilize a Dual Window-based Cross-Attention (DWCA) module to fuse the LiDAR and camera features into a unified BEV representation. The fused BEV feature maps are shared among the CAVs, and a 3D Convolutional Neural Network is applied to aggregate the features from the CAVs. Our CoBEVFusion framework was evaluated on the cooperative perception dataset OPV2V for two perception tasks: BEV semantic segmentation and 3D object detection. The results show that our DWCA LiDAR-camera fusion model outperforms perception models with single-modal data and state-of-the-art BEV fusion models. Our overall cooperative perception architecture, CoBEVFusion, also achieves comparable performance with other cooperative perception models.
A Web Application for Experimenting and Validating Remote Measurement of Vital Signs
Aug 21, 2022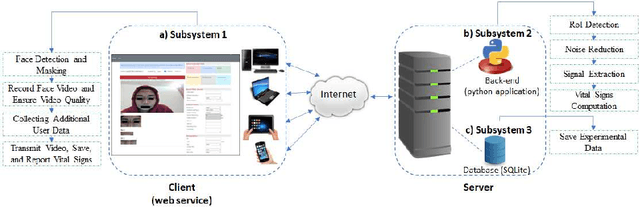

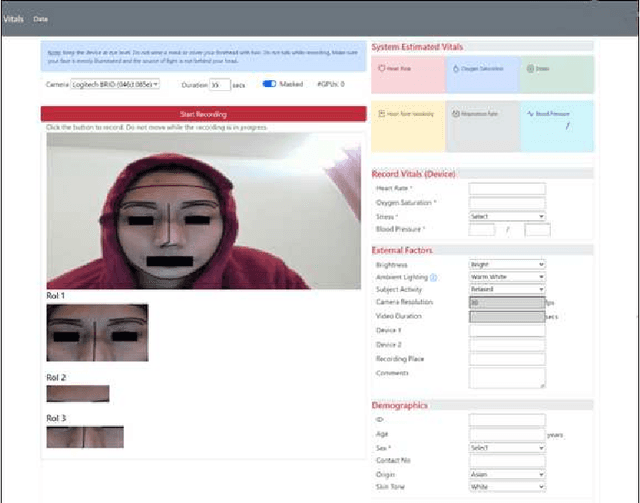
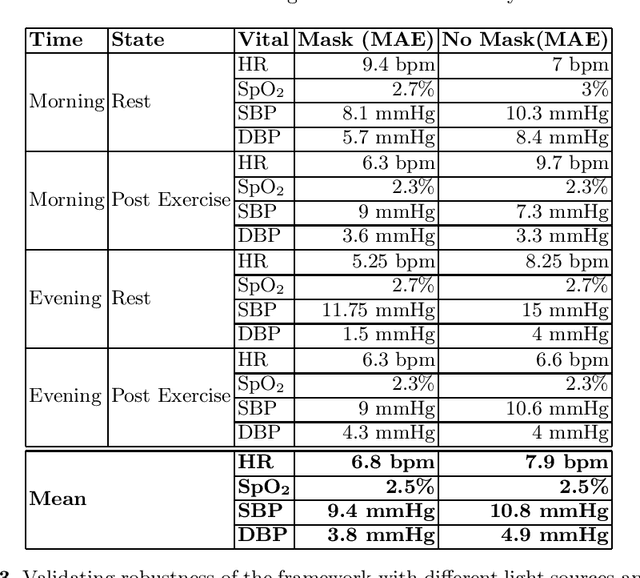
Abstract:With a surge in online medical advising remote monitoring of patient vitals is required. This can be facilitated with the Remote Photoplethysmography (rPPG) techniques that compute vital signs from facial videos. It involves processing video frames to obtain skin pixels, extracting the cardiac data from it and applying signal processing filters to extract the Blood Volume Pulse (BVP) signal. Different algorithms are applied to the BVP signal to estimate the various vital signs. We implemented a web application framework to measure a person's Heart Rate (HR), Heart Rate Variability (HRV), Oxygen Saturation (SpO2), Respiration Rate (RR), Blood Pressure (BP), and stress from the face video. The rPPG technique is highly sensitive to illumination and motion variation. The web application guides the users to reduce the noise due to these variations and thereby yield a cleaner BVP signal. The accuracy and robustness of the framework was validated with the help of volunteers.
ReViSe: Remote Vital Signs Measurement Using Smartphone Camera
Jun 13, 2022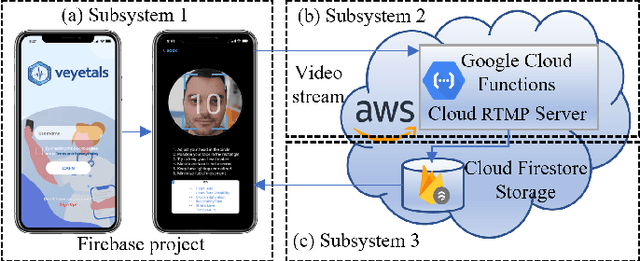
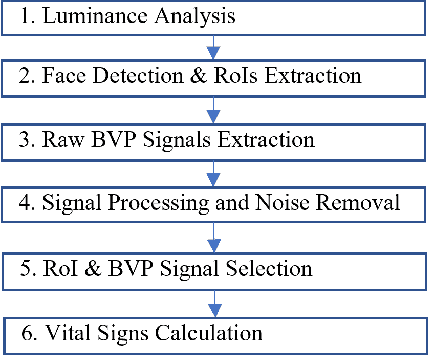
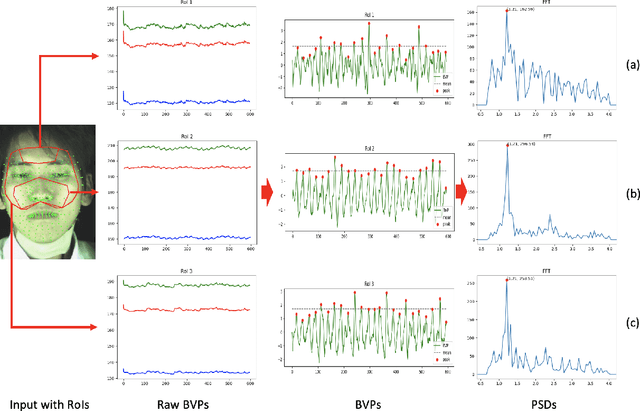
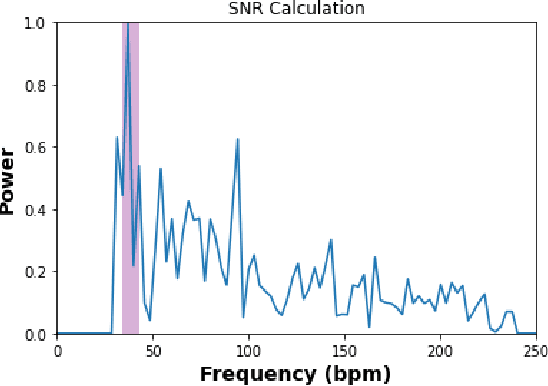
Abstract:Remote Photoplethysmography (rPPG) is a fast, effective, inexpensive and convenient method for collecting biometric data as it enables vital signs estimation using face videos. Remote contactless medical service provisioning has proven to be a dire necessity during the COVID-19 pandemic. We propose an end-to-end framework to measure people's vital signs including Heart Rate (HR), Heart Rate Variability (HRV), Oxygen Saturation (SpO2) and Blood Pressure (BP) based on the rPPG methodology from the video of a user's face captured with a smartphone camera. We extract face landmarks with a deep learning-based neural network model in real-time. Multiple face patches also called Region-of-Interests (RoIs) are extracted by using the predicted face landmarks. Several filters are applied to reduce the noise from the RoIs in the extracted cardiac signals called Blood Volume Pulse (BVP) signal. We trained and validated machine learning models using two public rPPG datasets namely the TokyoTech rPPG and the Pulse Rate Detection (PURE) datasets, on which our models achieved the following Mean Absolute Errors (MAE): a) for HR, 1.73 and 3.95 Beats-Per-Minute (bpm) respectively, b) for HRV, 18.55 and 25.03 ms respectively, and c) for SpO2, a MAE of 1.64 on the PURE dataset. We validated our end-to-end rPPG framework, ReViSe, in real life environment, and thereby created the Video-HR dataset. Our HR estimation model achieved a MAE of 2.49 bpm on this dataset. Since no publicly available rPPG datasets existed for BP measurement with face videos, we used a dataset with signals from fingertip sensor to train our model and also created our own video dataset, Video-BP. On our Video-BP dataset, our BP estimation model achieved a MAE of 6.7 mmHg for Systolic Blood Pressure (SBP), and a MAE of 9.6 mmHg for Diastolic Blood Pressure (DBP).
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge