David Wild
City-wide Analysis of Electronic Health Records Reveals Gender and Age Biases in the Administration of Known Drug-Drug Interactions
Mar 09, 2018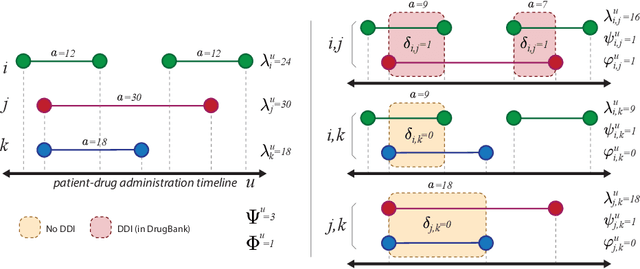



Abstract:From a public-health perspective, the occurrence of drug-drug-interactions (DDI) from multiple drug prescriptions is a serious problem, especially in the elderly population. This is true both for individuals and the system itself since patients with complications due to DDI will likely re-enter the system at a costlier level. We conducted an 18-month study of DDI occurrence in Blumenau (Brazil; pop. 340,000) using city-wide drug dispensing data from both primary and secondary-care level. Our goal is also to identify possible risk factors in a large population, ultimately characterizing the burden of DDI for patients, doctors and the public system itself. We found 181 distinct DDI being prescribed concomitantly to almost 5% of the city population. We also discovered that women are at a 60% risk increase of DDI when compared to men, while only having a 6% co-administration risk increase. Analysis of the DDI co-occurrence network reveals which DDI pairs are most associated with the observed greater DDI risk for females, demonstrating that contraception and hormone therapy are not the main culprits of the gender disparity, which is maximized after the reproductive years. Furthermore, DDI risk increases dramatically with age, with patients age 70-79 having a 50-fold risk increase in comparison to patients aged 0-19. Interestingly, several null models demonstrate that this risk increase is not due to increased polypharmacy with age. Finally, we demonstrate that while the number of drugs and co-administrations help predict a patient's number of DDI ($R^2=.413$), they are not sufficient to flag these patients accurately, which we achieve by training classifiers with additional data (MCC=.83,F1=.72). These results demonstrate that accurate warning systems for known DDI can be devised for public and private systems alike, resulting in substantial prevention of DDI-related ADR and savings.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge