Carri W. Chan
Robust Policies For Proactive ICU Transfers
Feb 14, 2020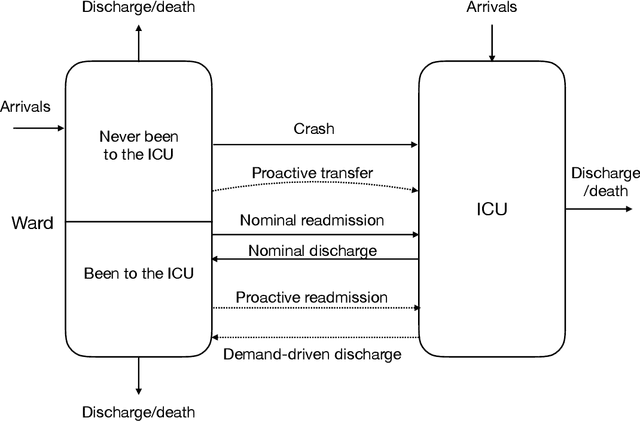
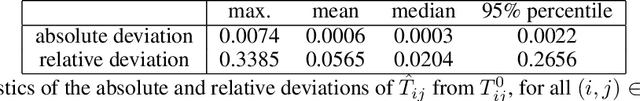
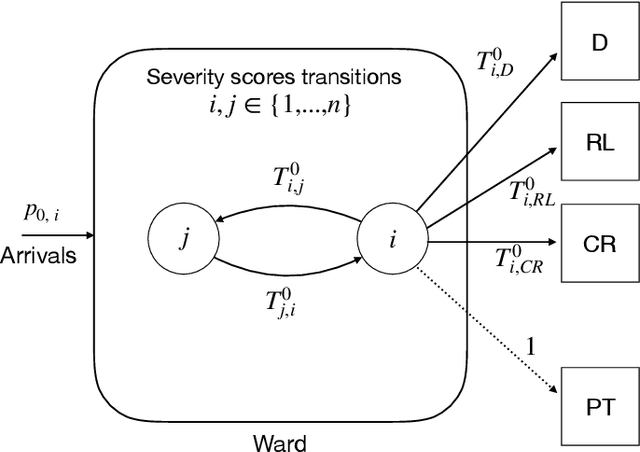
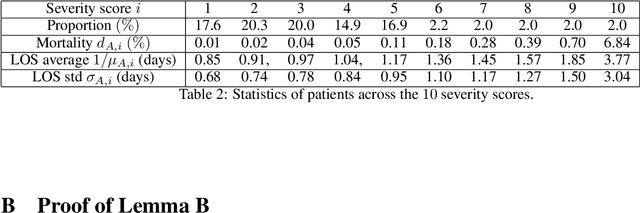
Abstract:Patients whose transfer to the Intensive Care Unit (ICU) is unplanned are prone to higher mortality rates than those who were admitted directly to the ICU. Recent advances in machine learning to predict patient deterioration have introduced the possibility of \emph{proactive transfer} from the ward to the ICU. In this work, we study the problem of finding \emph{robust} patient transfer policies which account for uncertainty in statistical estimates due to data limitations when optimizing to improve overall patient care. We propose a Markov Decision Process model to capture the evolution of patient health, where the states represent a measure of patient severity. Under fairly general assumptions, we show that an optimal transfer policy has a threshold structure, i.e., that it transfers all patients above a certain severity level to the ICU (subject to available capacity). As model parameters are typically determined based on statistical estimations from real-world data, they are inherently subject to misspecification and estimation errors. We account for this parameter uncertainty by deriving a robust policy that optimizes the worst-case reward across all plausible values of the model parameters. We show that the robust policy also has a threshold structure under fairly general assumptions. Moreover, it is more aggressive in transferring patients than the optimal nominal policy, which does not take into account parameter uncertainty. We present computational experiments using a dataset of hospitalizations at 21 KNPC hospitals, and present empirical evidence of the sensitivity of various hospital metrics (mortality, length-of-stay, average ICU occupancy) to small changes in the parameters. Our work provides useful insights into the impact of parameter uncertainty on deriving simple policies for proactive ICU transfer that have strong empirical performance and theoretical guarantees.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge