Brendan E. Odigwe
Application of Machine Learning in Early Recommendation of Cardiac Resynchronization Therapy
Sep 13, 2021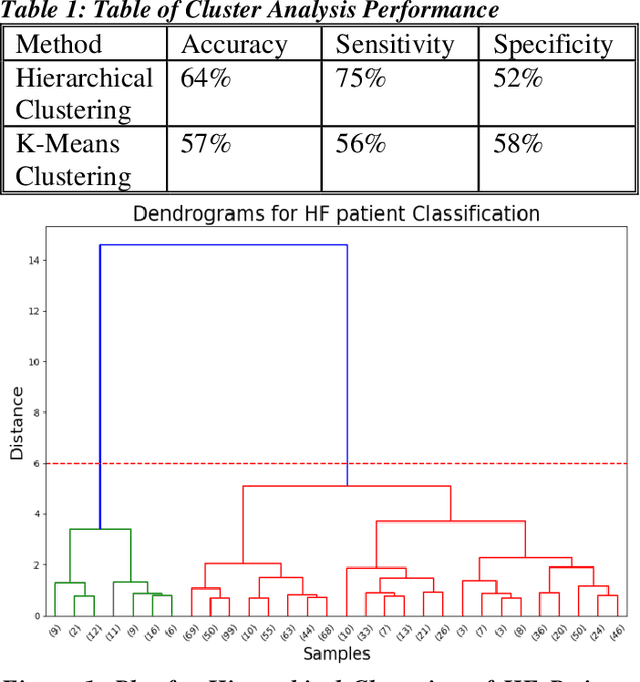
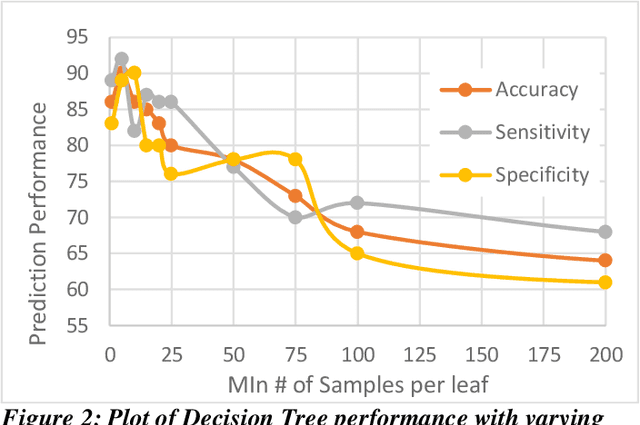
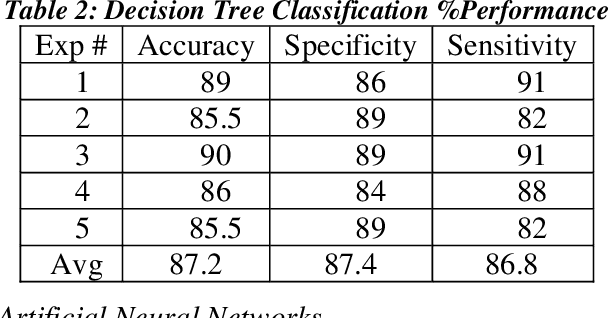
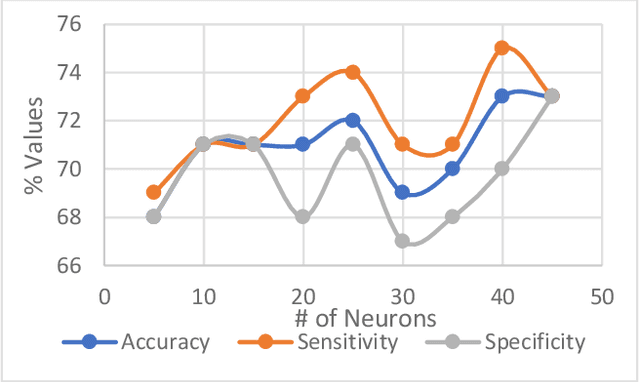
Abstract:Heart failure (HF) is a leading cause of morbidity, mortality, and health care costs. Prolonged conduction through the myocardium can occur with HF, and a device-driven approach, termed cardiac resynchronization therapy (CRT), can improve left ventricular (LV) myocardial conduction patterns. While a functional benefit of CRT has been demonstrated, a large proportion of HF patients (30-50%) receiving CRT do not show sufficient improvement. Moreover, identifying HF patients that would benefit from CRT prospectively remains a clinical challenge. Accordingly, strategies to effectively predict those HF patients that would derive a functional benefit from CRT holds great medical and socio-economic importance. Thus, we used machine learning methods of classifying HF patients, namely Cluster Analysis, Decision Trees, and Artificial neural networks, to develop predictive models of individual outcomes following CRT. Clinical, functional, and biomarker data were collected in HF patients before and following CRT. A prospective 6-month endpoint of a reduction in LV volume was defined as a CRT response. Using this approach (418 responders, 412 non-responders), each with 56 parameters, we could classify HF patients based on their response to CRT with more than 95% success. We have demonstrated that using machine learning approaches can identify HF patients with a high probability of a positive CRT response (95% accuracy), and of equal importance, identify those HF patients that would not derive a functional benefit from CRT. Developing this approach into a clinical algorithm to assist in clinical decision-making regarding the use of CRT in HF patients would potentially improve outcomes and reduce health care costs.
Modelling of Sickle Cell Anemia Patients Response to Hydroxyurea using Artificial Neural Networks
Nov 25, 2019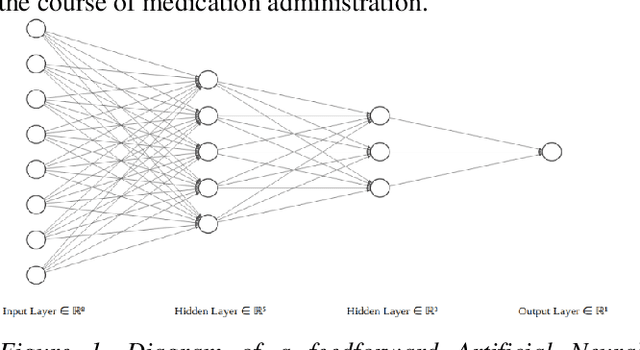
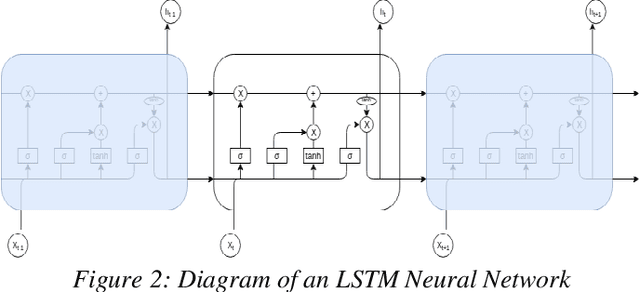
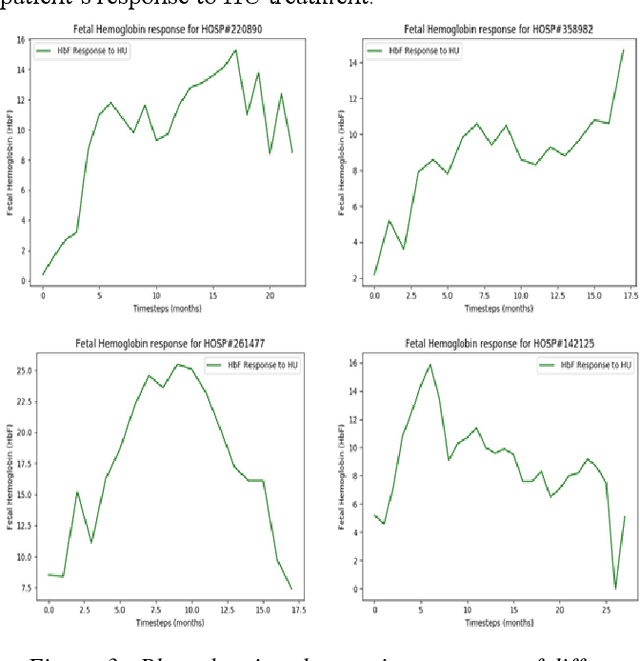
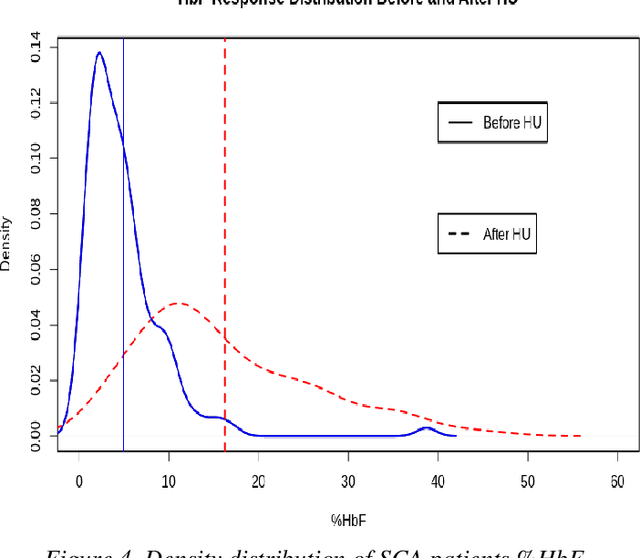
Abstract:Hydroxyurea (HU) has been shown to be effective in alleviating the symptoms of Sickle Cell Anemia disease. While Hydroxyurea reduces the complications associated with Sickle Cell Anemia in some patients, others do not benefit from this drug and experience deleterious effects since it is also a chemotherapeutic agent. Therefore, to whom, should the administration of HU be considered as a viable option, is the main question asked by the responsible physician. We address this question by developing modeling techniques that can predict a patient's response to HU and therefore spare the non-responsive patients from the unnecessary effects of HU on the values of 22 parameters that can be obtained from blood samples in 122 patients. Using this data, we developed Deep Artificial Neural Network models that can predict with 92.6% accuracy, the final HbF value of a subject after undergoing HU therapy. Our current studies are focussing on forecasting a patient's HbF response, 30 days ahead of time.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge