Predicting Breast Cancer Survival: A Survival Analysis Approach Using Log Odds and Clinical Variables
Paper and Code
Oct 17, 2024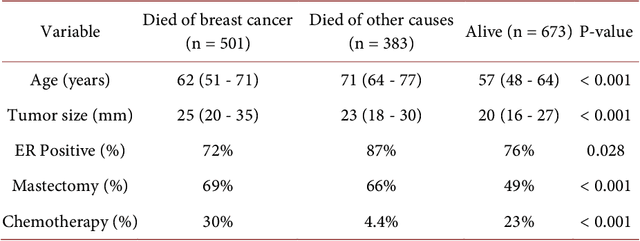
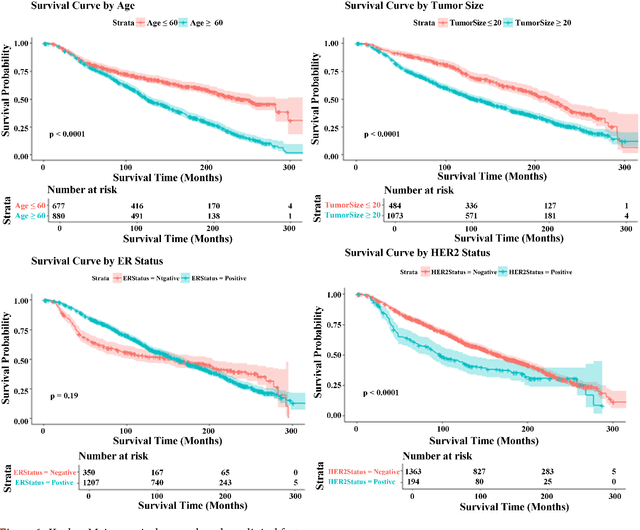
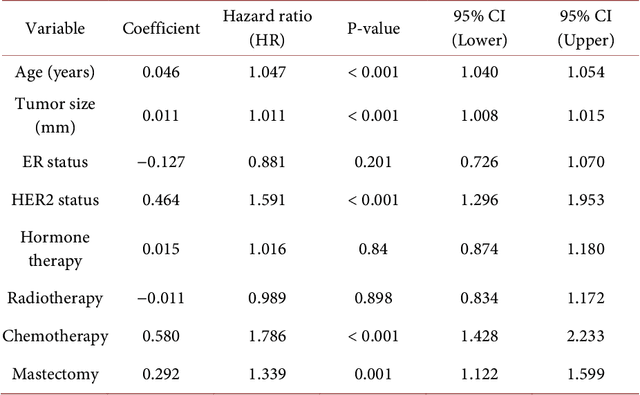
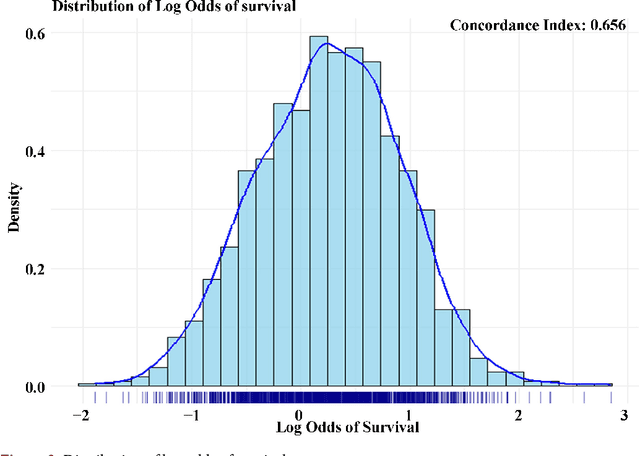
Breast cancer remains a significant global health challenge, with prognosis and treatment decisions largely dependent on clinical characteristics. Accurate prediction of patient outcomes is crucial for personalized treatment strategies. This study employs survival analysis techniques, including Cox proportional hazards and parametric survival models, to enhance the prediction of the log odds of survival in breast cancer patients. Clinical variables such as tumor size, hormone receptor status, HER2 status, age, and treatment history were analyzed to assess their impact on survival outcomes. Data from 1557 breast cancer patients were obtained from a publicly available dataset provided by the University College Hospital, Ibadan, Nigeria. This dataset was preprocessed and analyzed using both univariate and multivariate approaches to evaluate survival outcomes. Kaplan-Meier survival curves were generated to visualize survival probabilities, while the Cox proportional hazards model identified key risk factors influencing mortality. The results showed that older age, larger tumor size, and HER2-positive status were significantly associated with an increased risk of mortality. In contrast, estrogen receptor positivity and breast-conserving surgery were linked to better survival outcomes. The findings suggest that integrating these clinical variables into predictive models improvesthe accuracy of survival predictions, helping to identify high-risk patients who may benefit from more aggressive interventions. This study demonstrates the potential of survival analysis in optimizing breast cancer care, particularly in resource-limited settings. Future research should focus on integrating genomic data and real-world clinical outcomes to further refine these models.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge