Neurological Prognostication of Post-Cardiac-Arrest Coma Patients Using EEG Data: A Dynamic Survival Analysis Framework with Competing Risks
Paper and Code
Aug 17, 2023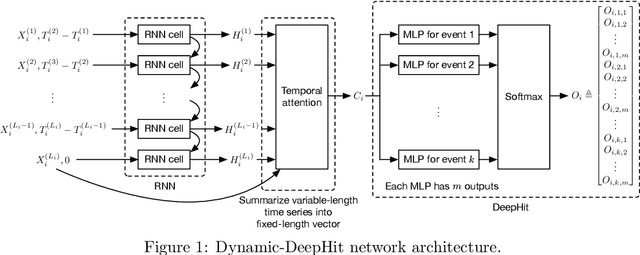
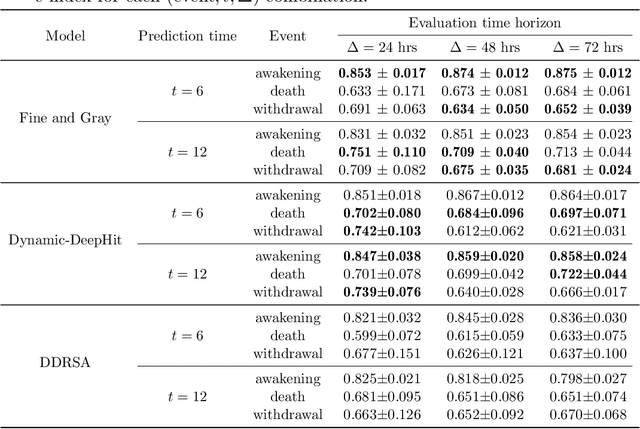
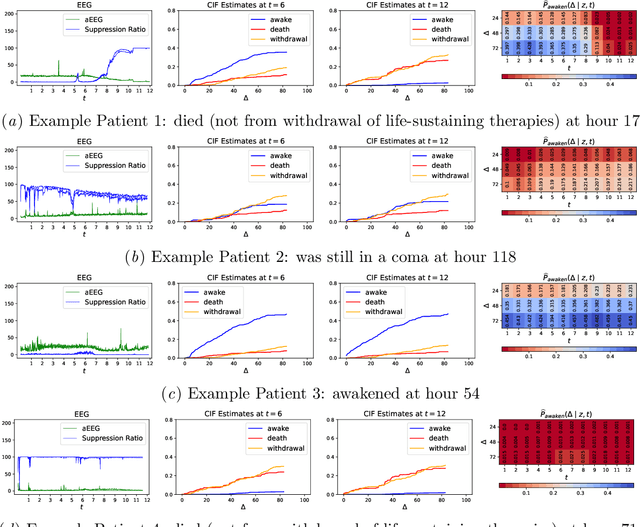

Patients resuscitated from cardiac arrest who enter a coma are at high risk of death. Forecasting neurological outcomes of these patients (the task of neurological prognostication) could help with treatment decisions. In this paper, we propose, to the best of our knowledge, the first dynamic framework for neurological prognostication of post-cardiac-arrest comatose patients using EEG data: our framework makes predictions for a patient over time as more EEG data become available, and different training patients' available EEG time series could vary in length. Predictions are phrased in terms of either time-to-event outcomes (time-to-awakening or time-to-death) or as the patient's probability of awakening or of dying across multiple time horizons. Our framework uses any dynamic survival analysis model that supports competing risks in the form of estimating patient-level cumulative incidence functions. We consider three competing risks as to what happens first to a patient: awakening, being withdrawn from life-sustaining therapies (and thus deterministically dying), or dying (by other causes). We demonstrate our framework by benchmarking three existing dynamic survival analysis models that support competing risks on a real dataset of 922 patients. Our main experimental findings are that: (1) the classical Fine and Gray model which only uses a patient's static features and summary statistics from the patient's latest hour's worth of EEG data is highly competitive, achieving accuracy scores as high as the recently developed Dynamic-DeepHit model that uses substantially more of the patient's EEG data; and (2) in an ablation study, we show that our choice of modeling three competing risks results in a model that is at least as accurate while learning more information than simpler models (using two competing risks or a standard survival analysis setup with no competing risks).
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge