Identifying Diabetic Patients with High Risk of Readmission
Paper and Code
Feb 12, 2016
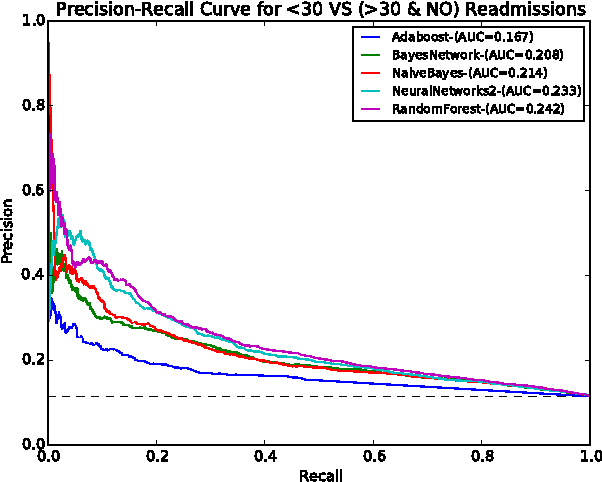
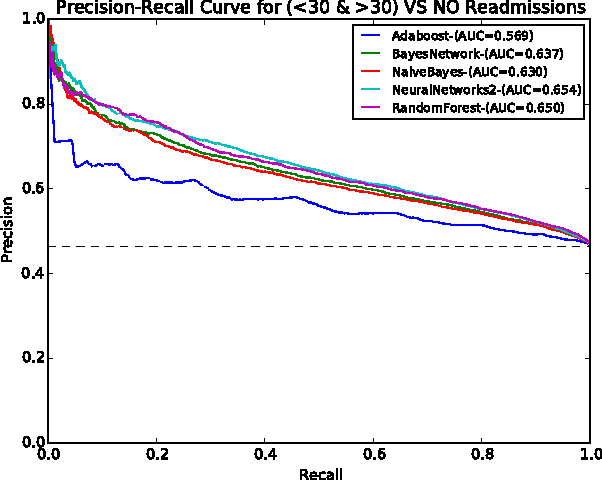
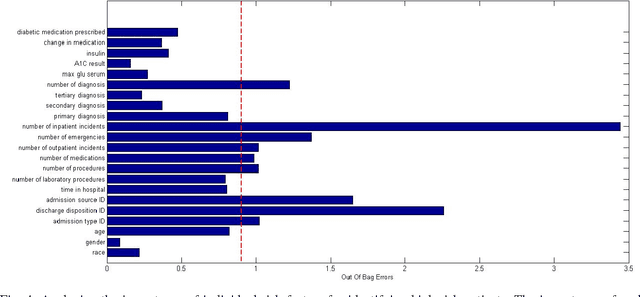
Hospital readmissions are expensive and reflect the inadequacies in healthcare system. In the United States alone, treatment of readmitted diabetic patients exceeds 250 million dollars per year. Early identification of patients facing a high risk of readmission can enable healthcare providers to to conduct additional investigations and possibly prevent future readmissions. This not only improves the quality of care but also reduces the medical expenses on readmission. Machine learning methods have been leveraged on public health data to build a system for identifying diabetic patients facing a high risk of future readmission. Number of inpatient visits, discharge disposition and admission type were identified as strong predictors of readmission. Further, it was found that the number of laboratory tests and discharge disposition together predict whether the patient will be readmitted shortly after being discharged from the hospital (i.e. <30 days) or after a longer period of time (i.e. >30 days). These insights can help healthcare providers to improve inpatient diabetic care. Finally, the cost analysis suggests that \$252.76 million can be saved across 98,053 diabetic patient encounters by incorporating the proposed cost sensitive analysis model.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge