Oleksandr Ivanov
Mednition Inc
Accurate detection of sepsis at ED triage using machine learning with clinical natural language processing
Apr 21, 2022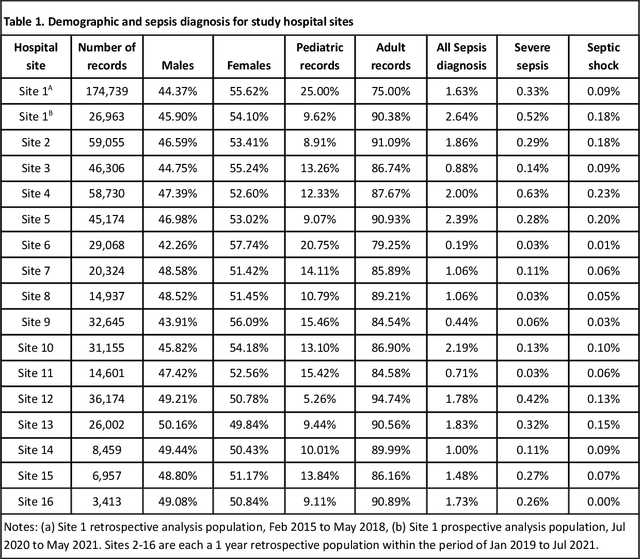
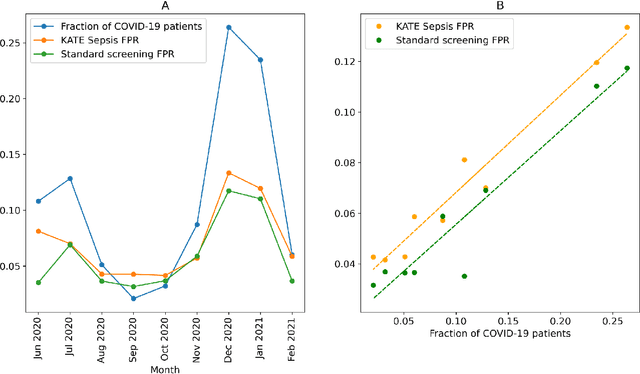
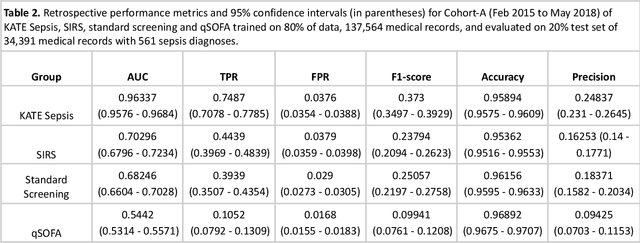
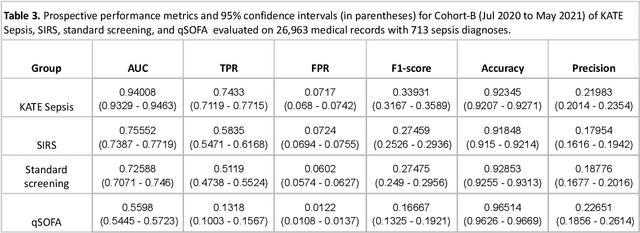
Abstract:Sepsis is a life-threatening condition with organ dysfunction and is a leading cause of death and critical illness worldwide. Accurate detection of sepsis during emergency department triage would allow early initiation of lab analysis, antibiotic administration, and other sepsis treatment protocols. The purpose of this study was to determine whether EHR data can be extracted and synthesized with the latest machine learning algorithms (KATE Sepsis) and clinical natural language processing to produce accurate sepsis models, and compare KATE Sepsis performance with existing sepsis screening protocols, such as SIRS and qSOFA. A machine learning model (KATE Sepsis) was developed using patient encounters with triage data from 16 participating hospitals. KATE Sepsis, SIRS, standard screening (SIRS with source of infection) and qSOFA were tested in three settings. Cohort-A was a retrospective analysis on medical records from a single Site 1. Cohort-B was a prospective analysis of Site 1. Cohort-C was a retrospective analysis on Site 1 with 15 additional sites. Across all cohorts, KATE Sepsis demonstrates an AUC of 0.94-0.963 with 73-74.87% TPR and 3.76-7.17% FPR. Standard screening demonstrates an AUC of 0.682-0.726 with 39.39-51.19% TPR and 2.9-6.02% FPR. The qSOFA protocol demonstrates an AUC of 0.544-0.56, with 10.52-13.18% TPR and 1.22-1.68% FPR. For severe sepsis, across all cohorts, KATE Sepsis demonstrates an AUC of 0.935-0.972 with 70-82.26% TPR and 4.64-8.62% FPR. For septic shock, across all cohorts, KATE Sepsis demonstrates an AUC of 0.96-0.981 with 85.71-89.66% TPR and 4.85-8.8% FPR. SIRS, standard screening, and qSOFA demonstrate low AUC and TPR for severe sepsis and septic shock detection. KATE Sepsis provided substantially better sepsis detection performance in triage than commonly used screening protocols.
Improving Emergency Department ESI Acuity Assignment Using Machine Learning and Clinical Natural Language Processing
Mar 29, 2020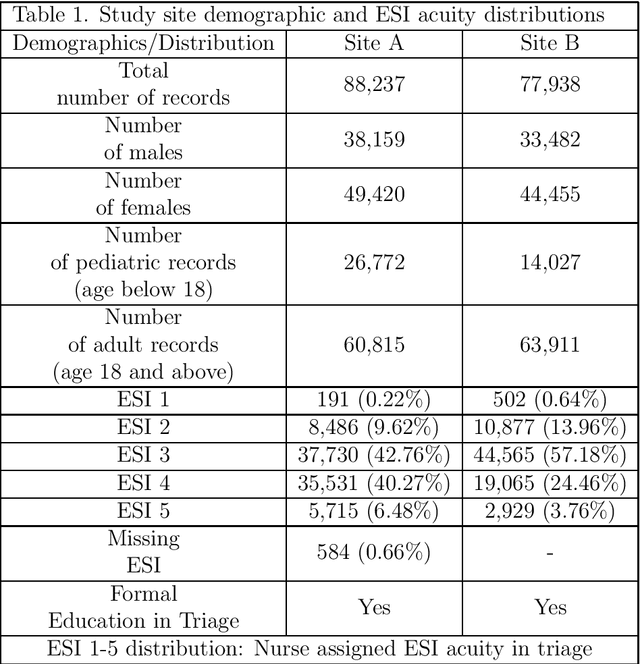
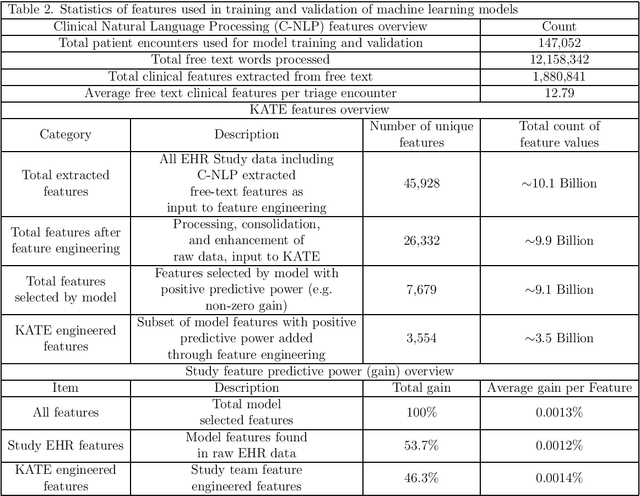
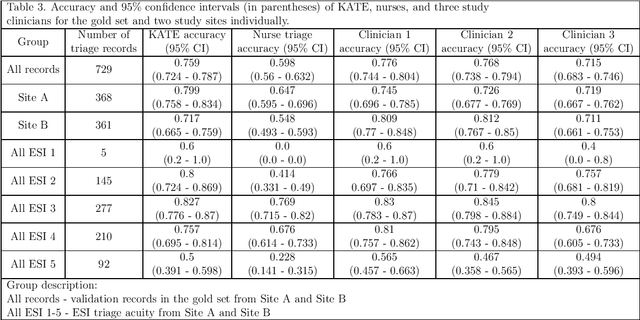
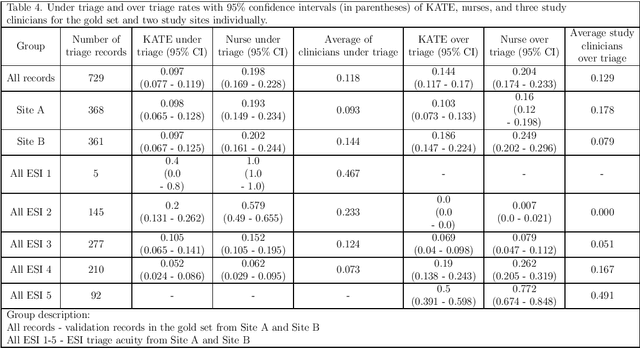
Abstract:Effective triage is critical to mitigating the effect of increased volume by accurately determining patient acuity, need for resources, and establishing effective acuity-based patient prioritization. The purpose of this retrospective study was to determine whether historical EHR data can be extracted and synthesized with clinical natural language processing (C-NLP) and the latest ML algorithms (KATE) to produce highly accurate ESI predictive models. An ML model (KATE) for the triage process was developed using 166,175 patient encounters from two participating hospitals. The model was then tested against a gold set that was derived from a random sample of triage encounters at the study sites and correct acuity assignments were recorded by study clinicians using the Emergency Severity Index (ESI) standard as a guide. At the two study sites, KATE predicted accurate ESI acuity assignments 75.9% of the time, compared to nurses (59.8%) and average individual study clinicians (75.3%). KATE accuracy was 26.9% higher than the average nurse accuracy (p-value < 0.0001). On the boundary between ESI 2 and ESI 3 acuity assignments, which relates to the risk of decompensation, KATE was 93.2% higher with 80% accuracy, compared to triage nurses with 41.4% accuracy (p-value < 0.0001). KATE provides a triage acuity assignment substantially more accurate than the triage nurses in this study sample. KATE operates independently of contextual factors, unaffected by the external pressures that can cause under triage and may mitigate the racial and social biases that can negatively affect the accuracy of triage assignment. Future research should focus on the impact of KATE providing feedback to triage nurses in real time, KATEs impact on mortality and morbidity, ED throughput, resource optimization, and nursing outcomes.
 Add to Chrome
Add to Chrome Add to Firefox
Add to Firefox Add to Edge
Add to Edge